2025-06-17 リンショーピング大学
<関連情報>
- https://liu.se/en/news-item/fettlever-men-inte-leverskada-vanligt-vid-typ-2-diabetes
- https://onlinelibrary.wiley.com/doi/10.1111/joim.20103
プライマリ・ケアにおける2型糖尿病患者における代謝機能障害関連脂肪性肝疾患の有病率と重症度の評価 Evaluating the prevalence and severity of metabolic dysfunction-associated steatotic liver disease in patients with type 2 diabetes mellitus in primary care
Wile Balkhed, Martin Bergram, Fredrik Iredahl, Markus Holmberg, Carl Edin, Carl-Johan Carlhäll, Tino Ebbers, Pontus Henriksson, Christian Simonsson, Karin Rådholm …
Journal of Internal Medicine Published: 16 June 2025
DOI:https://doi.org/10.1111/joim.20103
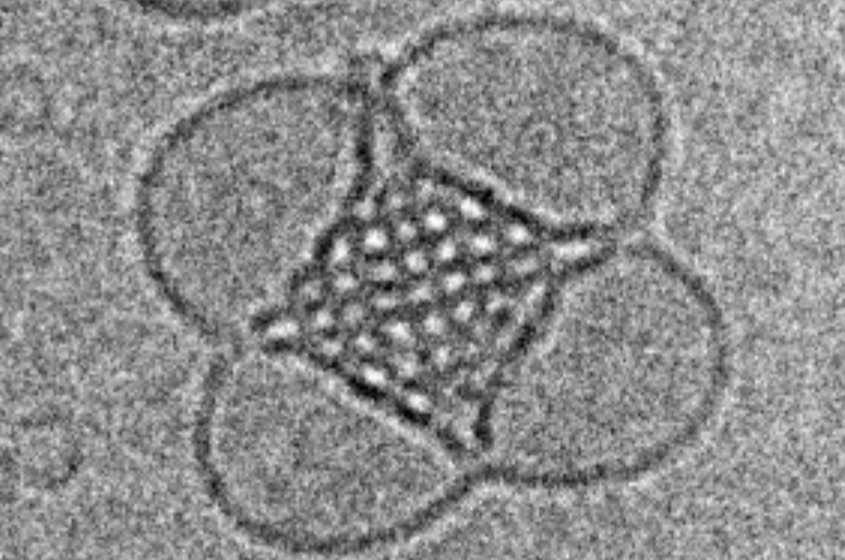
Graphical Abstract

Abstract
Background and aims
The prevalence of metabolic dysfunction-associated steatotic liver disease (MASLD) has increased during the epidemic of obesity. Type 2 diabetes mellitus (T2DM) is associated with progressive MASLD. Therefore, many guidelines recommend screening for MASLD in patients with T2DM. Most studies in patients with MASLD have been conducted in specialist care. We investigated the prevalence and severity of MASLD in patients with T2DM from primary care.
Methods
Patients with T2DM were prospectively included from primary care facilities to undergo transient elastography with controlled attenuation parameter and whole-body magnetic resonance imaging (MRI) to assess liver fat, cardiac function, muscle composition, and distribution of body fat.
Results
Among 308 participants, 59% had MASLD, 7% had suspected advanced fibrosis (transient elastography ≥ 10 kPa), and 1.9% had cirrhosis. The mean age was 63.9 ± 8.1 years; 37% were female, with no differences between the MASLD and the non-MASLD groups. Participants with MASLD had greater body mass index (31.1 ± 4.4 vs. 27.4 ± 4.1 kg/m2, p < 0.001) and a higher prevalence of obesity (60% vs. 21%, p < 0.001). Obesity increased the risk of fibrotic MASLD eightfold, as confirmed by multivariable analysis. Participants with MASLD also had increased visceral and abdominal subcutaneous adipose tissue and muscle fat infiltration. On cardiac MRI, participants with MASLD had a lower left ventricular (LV) stroke volume index, a lower LV end-diastolic volume index, and an increased LV concentricity.
Conclusions
In this cohort of primary care patients with T2DM, 59% had MASLD, and 7% had suspected advanced fibrosis. Obesity was a strong predictor of fibrotic MASLD. MASLD was associated with alterations to the left ventricle and increased deposition of ectopic fat.