2025-10-03 カロリンスカ研究所(KI)
<関連情報>
- https://news.ki.se/pots-common-in-patients-with-long-covid
- https://www.ahajournals.org/doi/10.1161/CIRCEP.124.013629
重症長期COVID-19患者における体位性起立性頻脈症候群の有病率と臨床的影響 Prevalence and Clinical Impact of Postural Orthostatic Tachycardia Syndrome in Highly Symptomatic Long COVID
Mikael Björnson, MD, Klara Wijnbladh, MD, Anna Törnberg, MSc, Anna Svensson-Raskh, RPT, PhD, Annie Svensson, MSc, RPT, Marcus Ståhlberg, MD, PhD, Michael Runold, MD, PhD, Artur Fedorowski, MD, PhD, Malin Nygren Bonnier, PT, PhD, and Judith Bruchfeld, MD, PhD
Circulation: Arrhythmia and Electrophysiology Published: 30 September 2025
DOI:https://doi.org/10.1161/CIRCEP.124.013629
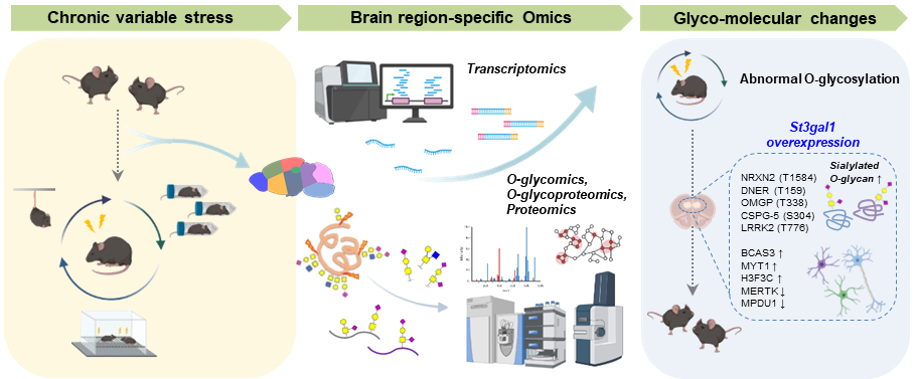
Graphical Abstract

Abstract
BACKGROUND:
The incidence of postural orthostatic tachycardia syndrome (POTS) in long COVID has been a growing concern since the first cases were reported in 2021. The aim of this study was to assess the prevalence and clinical impact of POTS in a series of well-characterized patients with long COVID.
METHODS:
We prospectively analyzed 467 nonhospitalized, highly symptomatic (sick leave ≥50%) patients with long COVID, and studied differences in demographics and clinical assessment outcomes between those diagnosed with POTS and the remaining long COVID patients. Examinations were performed at a median of 12 months after acute COVID-19, followed by a cardiologist evaluation with 48-hour ECG, head-up tilt test, and Active Stand Test for those with clinically suspected POTS.
RESULTS:
Of all long COVID patients, 143 (31%) were diagnosed with POTS, 128 (27%) did not fulfill POTS criteria, while 196 (42%) had no clinical signs of POTS. Patients with POTS were younger (mean age, 40.0 versus 44.0 versus 47.0 years, respectively; P≤0.001) and predominantly female (91%). They had significantly lower physical activity compared with the other 2 groups, as measured with the Frändin-Grimby scale (P=0.001). Heart rates during the 6-minute walk test were significantly higher in the POTS group, both during walking and at rest afterward, with a significantly shorter walking distance (448 m versus 472 m versus 509 m, respectively; P≤0.001). However, the distribution of symptoms showed no significant differences between the groups.
CONCLUSIONS:
In this cohort of predominantly younger women with highly symptomatic long COVID, POTS is common and presents with overlapping symptoms between POTS and non-POTS patients. Long COVID POTS confers lower physical activity and capacity compared with non-POTS long COVID and should be systematically assessed in this condition.