2025-11-19 東京科学大学
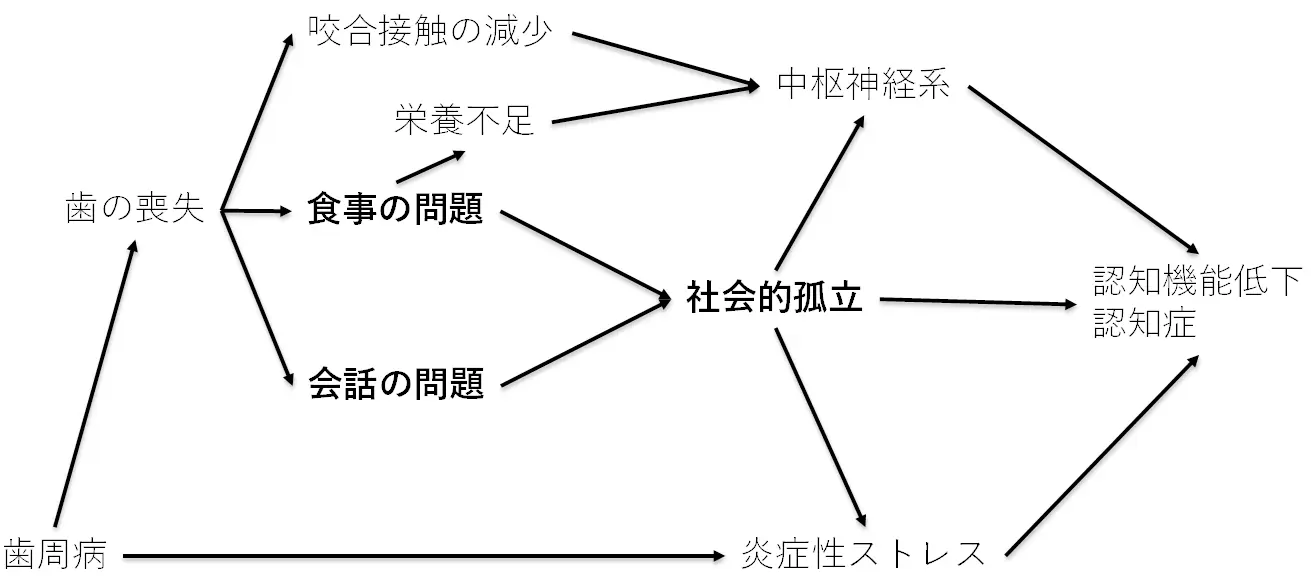
図1. 口腔の健康と認知症のメカニズムと、求められる研究手法
<関連情報>
- https://www.isct.ac.jp/ja/news/9g4w3kite9ah#top
- https://www.isct.ac.jp/plugins/cms/component_download_file.php?type=2&pageId=&contentsId=1&contentsDataId=2643&prevId=&key=6a289f2bb074458b2e4f13c6d5c6a028.pdf
- https://journals.sagepub.com/doi/10.1177/00220345251377014
- https://journals.sagepub.com/doi/10.1177/00220345251356437
口腔の健康と認知症:因果推論と理論的メカニズム Oral Health and Dementia: Causal Inference and Theoretical Mechanisms
J. Aida, S. Kiuchi, […], and Y. Matsuyama
Journal of Dental Research Published:October 18, 2025
DOI:https://doi.org/10.1177/00220345251377014
Abstract
Although studies have shown an association between oral health and dementia, causality and underlying mechanisms remain under debate. Reverse causality and unmeasured confounding factors, such as childhood cognitive function, raise questions about causality. Regarding theoretical mechanisms, essential oral functions such as eating and speaking are rarely discussed. The aim of this review was 2-fold: 1) to explain how recent epidemiologic studies tried to address these criticisms and 2) to suggest future research directions. To address reverse causality, studies used repeated surveys over time. Some studies considered the bidirectional relationship between oral health and dementia using appropriate methods. However, even in these studies, cognitive function prior to baseline was not incorporated. To infer the influence of unmeasured confounders, quantitative bias analysis using the E value is recommended, wherein the E value indicates the minimum strength of an unmeasured confounder needed to invalidate an observed association. Furthermore, methods that can ignore the effects of unmeasured confounding are good options, including fixed effect analysis and the instrumental variable method. However, few studies have applied these methods, yielding mixed results. Regarding mechanisms, although eating and speaking are essential oral functions, they have often been overlooked as potential mechanisms. These functions have a social aspect that facilitates interpersonal interactions and can reduce social isolation. The expert commission reported that social isolation in later life is 1 of the 14 modifiable risk factors for dementia. When we consider multilayered direct and indirect mechanisms of dementia throughout the life course in addition to the previously proposed mechanisms, such as periodontal inflammation, we find that poor oral health possibly increases dementia through social isolation via eating and speaking problems. In conclusion, based on causal inference studies and theoretical frameworks, oral health may be a modifiable risk factor for dementia. Methodologically and theoretically robust studies considering these points are needed to determine causality between oral health and dementia.
口腔虚弱は高齢日本人の体重減少の予測因子となる:コホート研究 Oral Frailty as a Predictor for Weight Loss in Older Japanese: A Cohort Study
K. Wang, Y. Matsuyama, […], and J. Aida
Journal of Dental Research Published:August 16, 2025
DOI:https://doi.org/10.1177/00220345251356437
Abstract
Oral frailty is a key factor in maintaining nutritional status, yet its impact on weight loss remains unclear. This study aimed to (1) evaluate the longitudinal association between oral frailty and the onset of weight loss among independent older adults and (2) explore how oral frailty components contribute to this association. Data were sourced from 2016 to 2022 of the Japan Gerontological Evaluation Study (JAGES). As a 6-y follow-up cohort study, the onset of >10% weight loss was used as the dependent variable, reflecting the significant threshold for older adults at ≥6-mo follow-up. Oral frailty was assessed as independent variables in 4 ways: (a) count score (sum of 5 components: fewer teeth, chewing difficulty, swallowing difficulty, dry mouth, and pronunciation difficulty), (b) individual 5 components, (c) a latent variable structured from 5 components, and (d) a refined latent variable incorporating additional paths from fewer teeth to chewing difficulty and pronunciation difficulty. Structural equation models (SEMs) were applied to examine the effect of oral frailty on weight loss, estimating standardized coefficients (SCs) and 95% confidence intervals (CIs). The construct validity of oral frailty was assessed using confirmatory factor analysis within the SEM framework. Model fit was evaluated using the standardized root mean squared residual (SRMR) and coefficient of determination (CD). Among 3,305 participants (47.4% women; mean age at baseline: 72.0 ± 4.9 y), 8.9% experienced >10% weight loss. Model d, which incorporated a refined latent structure of oral frailty, demonstrated the strongest association with weight loss (SC = 0.09; 95% confidence interval [CI] = 0.01; 0.16) among all models, with chewing difficulty showing the highest standardized factor loading (0.45; 95% CI = 0.35; 0.55). Model d also showed the best model fit (SRMR = 0.013; CD = 0.217), providing the high explanatory power and appropriateness of this model. Oral frailty significantly increases the risk of weight loss among independent older adults and its components have interrelationships.

