2025-07-09 カリフォルニア大学ロサンゼルス校 (UCLA)
<関連情報>
- https://newsroom.ucla.edu/stories/autoimmune-drug-reverses-immunotherapy-induced-diabetes-tests
- https://insight.jci.org/articles/view/188843
- https://www.science.org/doi/10.1126/scitranslmed.adg0675
多機能性T濾胞ヘルパー細胞がチェックポイント阻害型糖尿病を促進し、JAK阻害剤治療の標的となる Polyfunctional T follicular helper cells drive checkpoint-inhibitor diabetes and are targeted by JAK inhibitor therapy
Nicole L. Huang, Jessica G. Ortega, Kyleigh Kimbrell, Joah Lee, Lauren N. Scott, Esther M. Peluso, Sarah J. Wang, Ellie Y. Kao, Kristy Kim, Jarod Olay, Jaden N. Nguyen, Zoe Quandt, Trevor E. Angell, Maureen A. Su,and Melissa G. Lechner
JCI Insight Published: July 8, 2025
DOI:https://doi.org/10.1172/jci.insight.188843
Graphical Abstract

Abstract
Immune checkpoint inhibitors (ICI) have revolutionized cancer therapy, but their use is limited by the development of autoimmunity in healthy tissues as a side effect of treatment. Such immune-related adverse events (IrAE) contribute to hospitalizations, cancer treatment interruption, and even premature death. ICI-induced autoimmune diabetes mellitus (ICI-T1DM) is a life-threatening IrAE that presents with rapid pancreatic β-islet cell destruction leading to hyperglycemia and life-long insulin dependence. While prior reports have focused on CD8+ T cells, the role for CD4+ T cells in ICI-T1DM is less understood. We identify expansion of CD4+ T follicular helper (Tfh) cells expressing IL-21 and IFN-γ as a hallmark of ICI-T1DM. Furthermore, we show that both IL-21 and IFN-γ are critical cytokines for autoimmune attack in ICI-T1DM. Because IL-21 and IFN-γ both signal through JAK/STAT pathways, we reasoned that JAK inhibitors (JAKi) may protect against ICI-T1DM. Indeed, JAKi provide robust in vivo protection against ICI-T1DM in a mouse model that is associated with decreased islet-infiltrating Tfh cells. Moreover, JAKi therapy impaired Tfh cell differentiation in patients with ICI-T1DM. These studies highlight CD4+ Tfh cells as underrecognized but critical mediators of ICI-T1DM that may be targeted with JAKi to prevent this grave IrAE.
IL-21によってクローン状に増殖した甲状腺毒性エフェクターCD8+T細胞はチェックポイント阻害薬による甲状腺炎に寄与する Clonally expanded, thyrotoxic effector CD8+ T cells driven by IL-21 contribute to checkpoint inhibitor thyroiditis
Melissa G. Lechner, Zikang Zhou, Aline T. Hoang, Nicole Huang, […] , and Maureen A. Su
Science Translational Medicine Published:17 May 2023
DOI:https://doi.org/10.1126/scitranslmed.adg0675
Investigating IRAEs
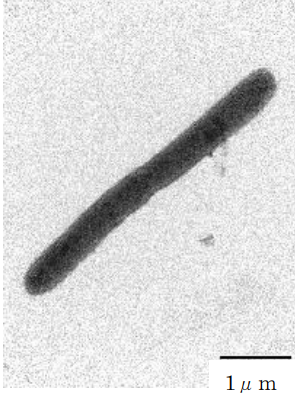
Immune related adverse events (IRAEs) occur in up to 60% of patients treated with immune checkpoint inhibitors (ICIs). A common IRAE is ICI-thyroiditis, which can result in destruction of thyroid tissue and the need for thyroid hormone replacement therapy. Here, Lechner et al. compared the phenotypes of thyroid-infiltrating immune cells isolated from individuals with ICI-thyroiditis, individuals with Hashimoto’s thyroiditis, and controls without thyroid disease. ICI-thyroiditis was characterized by IL-21–producing T follicular helper (Tfh) and T peripheral helper (Tph) cells that drove expansion and cytotoxic activity of thyroid-infiltrating effector CD8+ T cells. These populations, which were similarly present in a mouse model of ICI-thyroiditis, could therefore represent therapeutic targets for this common IRAE. —CM
Abstract
Autoimmune toxicity occurs in up to 60% of patients treated with immune checkpoint inhibitor (ICI) therapy for cancer and represents an increasing clinical challenge for expanding the use of these treatments. To date, human immunopathogenic studies of immune-related adverse events (IRAEs) have relied on sampling of circulating peripheral blood cells rather than affected tissues. Here, we directly obtained thyroid specimens from individuals with ICI-thyroiditis, one of the most common IRAEs, and compared immune infiltrates with those from individuals with spontaneous autoimmune Hashimoto’s thyroiditis (HT) or no thyroid disease. Single-cell RNA sequencing revealed a dominant, clonally expanded population of thyroid-infiltrating cytotoxic CXCR6+ CD8+ T cells (effector CD8+ T cells) present in ICI-thyroiditis but not HT or healthy controls. Furthermore, we identified a crucial role for interleukin-21 (IL-21), a cytokine secreted by intrathyroidal T follicular (TFH) and T peripheral helper (TPH) cells, as a driver of these thyrotoxic effector CD8+ T cells. In the presence of IL-21, human CD8+ T cells acquired the activated effector phenotype with up-regulation of the cytotoxic molecules interferon-γ (IFN-γ) and granzyme B, increased expression of the chemokine receptor CXCR6, and thyrotoxic capacity. We validated these findings in vivo using a mouse model of IRAEs and further demonstrated that genetic deletion of IL-21 signaling protected ICI-treated mice from thyroid immune infiltration. Together, these studies reveal mechanisms and candidate therapeutic targets for individuals who develop IRAEs.