2025-12-18 国立がん研究センター,東京大学,東京都立駒込病院,九州がんセンター

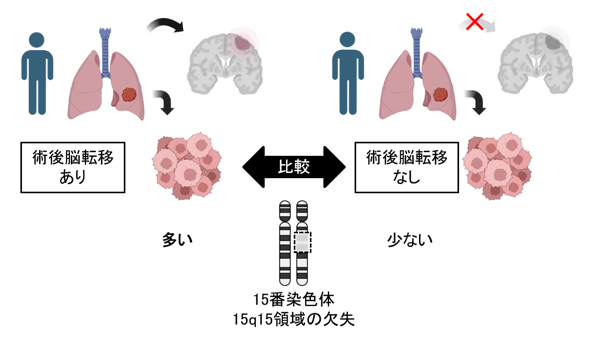
図1:遺伝子ごとに、病的バリアントの検出率とGermline conversion rateが大きく異なっていました。
<関連情報>
- https://www.ncc.go.jp/jp/information/researchtopics/2025/1218_2/index.html
- https://www.ncc.go.jp/jp/information/researchtopics/2025/1218_2/20251218_2.pdf
- https://aacrjournals.org/clincancerres/article-abstract/doi/10.1158/1078-0432.CCR-25-2985/770966/Germline-pathogenic-variant-prediction-model-for
日本の臨床ゲノムデータベースに基づく腫瘍のみのシーケンスのための生殖細胞病原性変異予測モデル Germline pathogenic variant prediction model for tumor-only sequencing based on Japanese clinicogenomic database
Masachika Ikegami;Liuzhe Zhang;Makoto Hirata;Tatsuro Yamaguchi;Shinya Oda;Shinji Kohsaka;Hiroyuki Mano;Toshihide Hirai;Hiroshi Kobayashi
Clinical Cancer Research Published:December 17 2025
DOI:https://doi.org/10.1158/1078-0432.CCR-25-2985
Abstract
Purpose: Germline pathogenic variants (GPVs) are frequently identified as secondary findings in cancer gene panel testing. Due to limited data on germline conversion rates (GCRs) in the Japanese population, clinical decisions have relied on ESMO criteria. We aimed to develop a variant-level GCR prediction algorithm using Japanese tumor-normal matched panel database and compare its utility with existing standards. Patients and Methods: We analyzed 7,078 Japanese cases from the NCC Oncopanel dataset, focusing on 32 hereditary cancer genes. Clinical features, sample information, sequence results, and minor allele frequency (MAF) in healthy populations were incorporated int a machine learning model and nomogram. Clinical utility was assessed via decision curve analysis and validated using GenMineTOP dataset. Results: Among 3,372 cases (mean age 61; 51% male), 4,905 pathogenic variants were identified, including 491 GPVs (GCR: 10%). High disease-specific GCRs were observed in BAP1 (11% in ocular tumors), BRCA1 and/or BRCA2 (13–16% in ovarian/peritoneal cancers), and NF1 (16% in peripheral nerve tumors). Genes with >50% GCRs included RAD51C, BRCA1, PALB2, CHEK2, RET, BRCA2, and PMS2. Significant predictors included age <30, multiple cancers, gene type, cancer type, MAF, relative variant allele frequency to tumor purity, and tumor allele ratio (TAR). The model achieved a c-index of 0.96–0.97, outperforming ESMO (0.88), with a 1.2% net benefit at a 5% threshold. The results were confirmed using GenMineTOP dataset. Conclusions: Variant-level prediction models for Japanese cancer patients incorporating TAR and MAF offer improved GPV prediction over gene-level approaches and support clinical decision-making and personalized medicine.