2026-02-05 東京科学大学
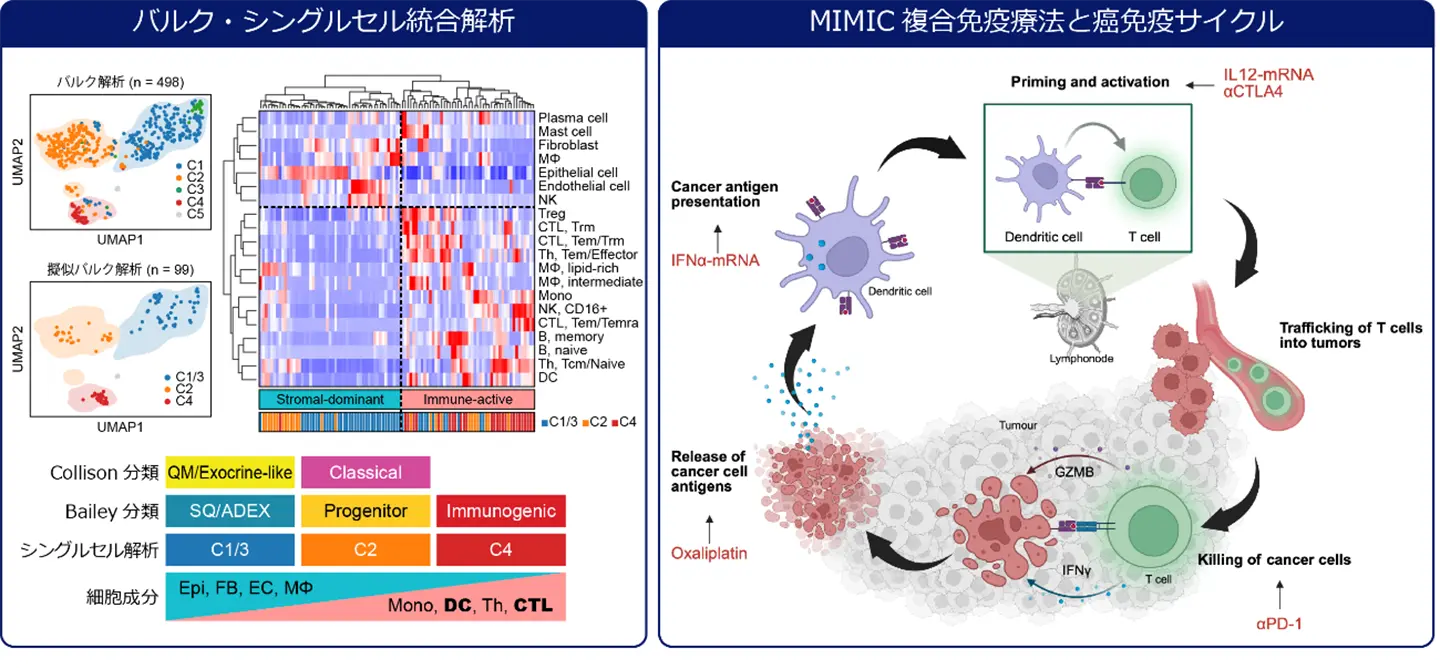
図1. バルク・シングルセル統合解析による膵癌の免疫組織学的分類(左)と、各段階において抗癌剤、免疫チェックポイント阻害剤、ならびにサイトカイン誘導性mRNA医薬で介入することにより、癌免疫サイクルを駆動する複合免疫療法MIMICの概要(右)
<関連情報>
- https://www.isct.ac.jp/ja/news/rtlv6q5b06u9
- https://www.isct.ac.jp/plugins/cms/component_download_file.php?type=2&pageId=&contentsId=1&contentsDataId=3148&prevId=&key=96c5da71ab1be8d2cb7b6c781590ea4d.pdf
- https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(26)00018-6/fulltext
サイトカインmRNAベースの治療は、前臨床マウスモデルにおいて樹状細胞とT細胞の不足を軽減し、悪性膵臓癌を排除する Cytokine mRNA-based therapy alleviates dendritic cell and T cell paucity to eliminate aggressive pancreatic cancer in preclinical mouse models
Yoshiaki Tanji ∙ Shu Shimada ∙ Megumi Kato ∙ Yoshimitsu Akiyama ∙ Megumi Hatano ∙ Shu Tsukihara ∙ et al.eBioMedicine Published: February 3, 2026
DOI:https://doi.org/10.1016/j.ebiom.2026.106137
Summary
Background
Pancreatic ductal adenocarcinoma (PDAC) with peritoneal dissemination is highly refractory to chemotherapy and immunotherapy, leading to poor prognosis. We aimed to develop an innovative therapeutic approach for advanced PDAC.
Methods
We performed comprehensive analyses of 498 bulk and 99 single-cell RNA-sequencing datasets. We established a syngeneic mouse model for subcutaneous and intraperitoneal metastatic tumours using mouse KrasG12D; Trp53R172H PDAC cells. A multimodal immunotherapy with mRNA-induced cytokines (MIMIC), that is, oxaliplatin, anti-PD-1 and anti-CTLA-4 antibodies, and intratumoural administration of mRNA therapeutics encoding interferon-α and interleukin-12, was evaluated in this preclinical model.
Findings
The aggressive PDAC subtype exhibited a paucity of dendritic cells (DCs) and T cells, causing an immunosuppressive tumour microenvironment. The syngeneic mouse model recapitulated this immunological phenotype with resistance to conventional systemic therapies. The MIMIC therapy not only significantly reduced the local tumour burden but also elicited a robust abscopal effect, suppressing distant peritoneal metastases and prolonging survival (P < 0.001). The omission of any single agent from the MIMIC regimen substantially abrogated the therapeutic efficacy. Flow cytometry and immunohistochemical analyses revealed that the MIMIC treatment enhanced immunogenic cell death, increased peripheral CD44+ CD62L- effector memory T cells, induced intratumoural infiltration of CD11c+ DCs and CD8+ T cells, and expanded TCR repertoire diversity.
Interpretation
Combining cytokine mRNA immunotherapy with cytotoxic killing and immune checkpoint blockade can reactivate antitumour immunity, offering a promising strategy for treating advanced PDAC.
Funding
This work was supported by Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT), Japan Agency for Medical Research and Development (AMED), and the Princess Takamatsu Cancer Research Fund.