血圧を下げる薬は、朝でも夜でも同じように効果があることが、大規模な臨床試験で明らかになりました。 Medication that lowers blood pressure is equally effective if taken in the morning or evening, a large clinical trial has found.
2022-10-17 エディンバラ大学
試験参加者は、少なくとも1種類の血圧を下げる薬を服用していた。半数は夜に、残りの半数は朝に薬を飲むように指示された。
試験参加者を5年間追跡調査した結果、心臓発作や脳卒中、循環器系の病気にかかった人の数は、朝のグループ362人に対し、夜のグループ390人と差がないことが判明した。
<関連情報>
- https://www.ed.ac.uk/news/2022/blood-pressure-medication-effective-at-any-time-of
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)01786-X/fulltext
英国における通常の高血圧治療薬の夜間投与と朝方投与による成人高血圧患者の心血管アウトカム(TIME study):前向き無作為化非盲検エンドポイント臨床試験 Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial
Isla S Mackenzie, Amy Rogers, Neil R Poulter, Bryan Williams,Morris J Brown, David J Webb, Ian Ford,David A Rorie,Greg Guthrie,J W Kerr Grieve, Filippo Pigazzani, Peter M Rothwell,Robin Young,Alex McConnachie, Allan D Struthers, Chim C Lang, Thomas M MacDonald, on behalf of theTIME Study Group
The Lancet Published:October 11, 2022
DOI:https://doi.org/10.1016/S0140-6736(22)01786-X

Summary
Background
Studies have suggested that evening dosing with antihypertensive therapy might have better outcomes than morning dosing. The Treatment in Morning versus Evening (TIME) study aimed to investigate whether evening dosing of usual antihypertensive medication improves major cardiovascular outcomes compared with morning dosing in patients with hypertension.
Methods
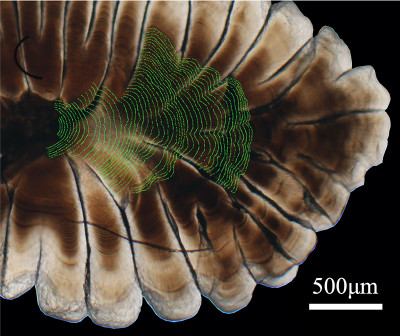
The TIME study is a prospective, pragmatic, decentralised, parallel-group study in the UK, that recruited adults (aged ≥18 years) with hypertension and taking at least one antihypertensive medication. Eligible participants were randomly assigned (1:1), without restriction, stratification, or minimisation, to take all of their usual antihypertensive medications in either the morning (0600–1000 h) or in the evening (2000–0000 h). Participants were followed up for the composite primary endpoint of vascular death or hospitalisation for non-fatal myocardial infarction or non-fatal stroke. Endpoints were identified by participant report or record linkage to National Health Service datasets and were adjudicated by a committee masked to treatment allocation. The primary endpoint was assessed as the time to first occurrence of an event in the intention-to-treat population (ie, all participants randomly assigned to a treatment group). Safety was assessed in all participants who submitted at least one follow-up questionnaire. The study is registered with EudraCT (2011-001968-21) and ISRCTN (18157641), and is now complete.
Findings
Between Dec 17, 2011, and June 5, 2018, 24 610 individuals were screened and 21 104 were randomly assigned to evening (n=10 503) or morning (n=10 601) dosing groups. Mean age at study entry was 65·1 years (SD 9·3); 12 136 (57·5%) participants were men; 8968 (42·5%) were women; 19 101 (90·5%) were White; 98 (0·5%) were Black, African, Caribbean, or Black British (ethnicity was not reported by 1637 [7·8%] participants); and 2725 (13·0%) had a previous cardiovascular disease. By the end of study follow-up (March 31, 2021), median follow-up was 5·2 years (IQR 4·9–5·7), and 529 (5·0%) of 10 503 participants assigned to evening treatment and 318 (3·0%) of 10 601 assigned to morning treatment had withdrawn from all follow-up. A primary endpoint event occurred in 362 (3·4%) participants assigned to evening treatment (0·69 events [95% CI 0·62–0·76] per 100 patient-years) and 390 (3·7%) assigned to morning treatment (0·72 events [95% CI 0·65–0·79] per 100 patient-years; unadjusted hazard ratio 0·95 [95% CI 0·83–1·10]; p=0·53). No safety concerns were identified.
Interpretation
Evening dosing of usual antihypertensive medication was not different from morning dosing in terms of major cardiovascular outcomes. Patients can be advised that they can take their regular antihypertensive medications at a convenient time that minimises any undesirable effects.
Funding
British Heart Foundation.