2023-04-04 バーミンガム大学
この研究が、国立医療技術評価機構(NICE)による新しいガイドラインに反映され、最大細胞減少手術を定期的に行う施設で治療を受けた患者の全生存率が向上することが示されました。
また、手術後12か月後のについても、手術の種類にかかわらず同じであることが示されました。
<関連情報>
- https://www.birmingham.ac.uk/news/2023/ovarian-cancer-surgery-birmingham-research-informs-new-guidance
- https://www.mdpi.com/2072-6694/14/18/4362
英国の多施設共同研究における人口ベースのデータを用いた進行卵巣癌の生存率に対する超急性期手術の影響の検討 Investigating the Impact of Ultra-Radical Surgery on Survival in Advanced Ovarian Cancer Using Population-Based Data in a Multicentre UK Study
Carole Cummins,Satyam Kumar,Joanna Long,Janos Balega,Tim Broadhead,Timothy Duncan,Richard J. Edmondson,Christina Fotopoulou,Rosalind M. Glasspool,Desiree Kolomainen,Simon Leeson,Ranjit Manchanda,Jo Morrison,Raj Naik,John A. Tidy,Nick Wood and Sudha Sundar
Cancers Published: 7 September 2022
DOI:https://doi.org/10.3390/cancers14184362
Simple Summary
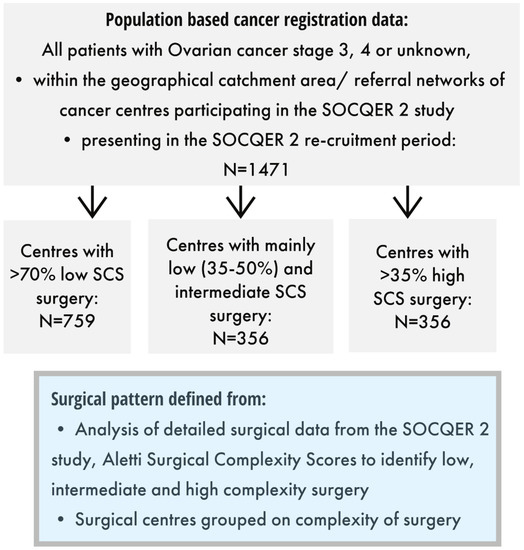
Ovarian cancer is treated by surgery to remove all visible cancer and chemotherapy. Cancer survival is highest when no cancer is left behind after surgery. Ultra-radical (URS) surgery or maximal effort cytoreduction surgery uses additional surgical procedures, e.g., splenectomy, diaphragm stripping, etc. to remove all visible cancer. The use of URS varies internationally with some cancer centres performing this routinely and others not. We conducted a multi-centre study investigating 1471 patients with advanced ovarian cancer (AOC) across three types of gynaecological cancer centres in the UK—those offering mainly low, intermediate or high complexity surgery and investigated survival from cancer in an operated and non-operated whole cohort of women with advanced ovarian cancer. We found that cancer survival was highest in the centres practicing more radical surgery, even after age and deprivation of patients was taken into consideration. Centres practicing mainly low complexity surgery should change practice.
Abstract
We investigated URS and impact on survival in whole patient cohorts with AOC treated within gynaecological cancer centres that participated in the previously presented SOCQER 2 study. National cancer registry datasets were used to identify FIGO Stage 3,4 and unknown stage patients from 11 cancer centres that had previously participated in the SOCQER2 study. Patient outcomes’ association with surgical ethos were evaluated using logistic regression and Cox proportional hazards. Centres were classified into three groups based on their surgical complexity scores (SCS); those practicing mainly low complexity, (5/11 centres with >70% low SCS procedures, 759 patients), mainly intermediate (3/11, 35–50% low SCS, 356 patients), or mainly high complexity surgery (3/11, >35% high SCS, 356 patients). Surgery rates were 43.2% vs. 58.4% vs. 60.9%. across mainly low, intermediate and high SCS centres, respectively, p < 0.001. Combined surgery and chemotherapy rates were 39.2% vs. 51.8% vs. 38.3% p < 0.000 across mainly low, intermediate and high complexity groups, respectively. Median survival was 23.1 (95% CI 19.0 to 27.2) vs. 22.0 (95% CI 17.6 to 26.3) vs. 17.9 months (95% CI 15.7 to 20.1), p = 0.043 in mainly high SCS, intermediate, and low SCS centres, respectively. In an age and deprivation adjusted model, compared to patients in the high SCS centres, patients in the low SCS group had an HR of 1.21 (95% CI 1.03 to 1.40) for death. Mainly high/intermediate SCS centres have significantly higher surgery rates and better survival at a population level. Centres that practice mainly low complexity surgery should change practice. This study provides support for the utilization of URS for patients with advanced OC.