リアルタイム技術により、3次元人工足場内の生きた細胞数を非侵襲的にカウントする。 Real-time technique noninvasively counts the number of live cells in a 3D artificial scaffold.
2023-05-05 米国国立標準技術研究所(NIST)
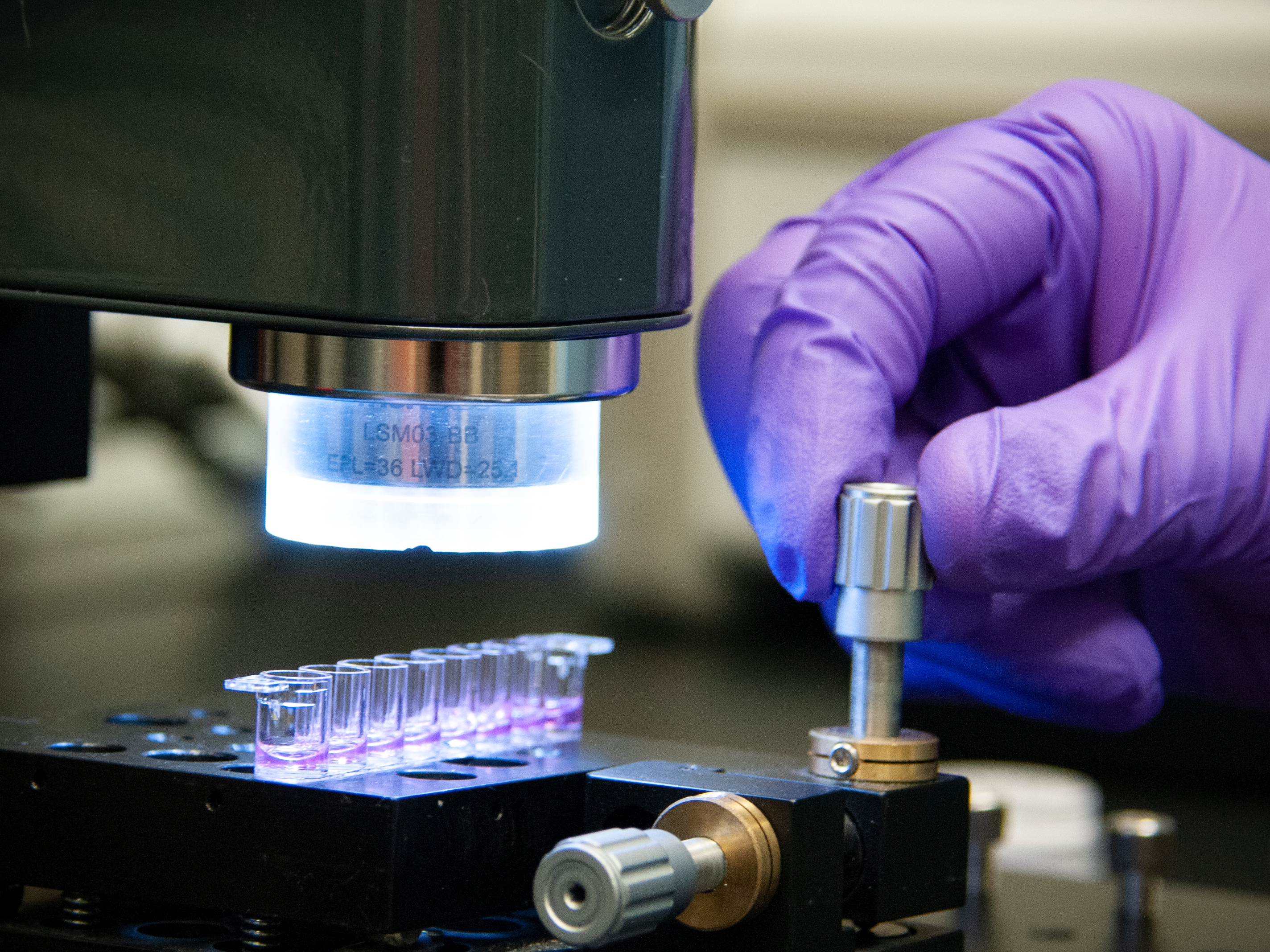 Researchers used a noninvasive and label-free method called optical coherence tomography to assess the live cells in the 3D scaffold system. OCT is an imaging technique that uses light waves to take cross sectional images of a sample.
Researchers used a noninvasive and label-free method called optical coherence tomography to assess the live cells in the 3D scaffold system. OCT is an imaging technique that uses light waves to take cross sectional images of a sample.
Credit: R. Wilson/NIST
◆米国の研究者らは、三次元支持体内の生きた細胞を数えるための侵襲性のない方法を開発し、それを評価するために光コヒーレンストモグラフィー(OCT)を使用した。新しい方法は、数時間から数分に減らし、部品の分解や破壊をすることなく、細胞の数と配置を監視することができるため、組織工学分野において未解決のニーズを満たしている。
<関連情報>
- https://www.nist.gov/news-events/news/2023/05/nist-develops-new-nondestructive-method-assessing-bioengineered-artificial
- https://onlinelibrary.wiley.com/doi/abs/10.1002/jbm.a.37528
光コヒーレンストモグラフィーを用いた組織工学用足場における3次元のラベルフリー細胞生存率計測 Three-dimensional, label-free cell viability measurements in tissue engineering scaffolds using optical coherence tomography
Greta Babakhanova, Anant Agrawal, Deepika Arora, Allison Horenberg, Jagat B. Budhathoki, Joy P. Dunkers, Joe Chalfoun, Peter Bajcsy, Carl G. Simon Jr
Journal of Biomedical Materials Research Part A Published: 14 March 2023
DOI:https://doi.org/10.1002/jbm.a.37528
Abstract
In the field of tissue engineering, 3D scaffolds and cells are often combined to yield constructs that are used as therapeutics to repair or restore tissue function in patients. Viable cells are often required to achieve the intended mechanism of action for the therapy, where the live cells may build new tissue or may release factors that induce tissue regeneration. Thus, there is a need to reliably measure cell viability in 3D scaffolds as a quality attribute of a tissue-engineered medical product. Here, we developed a noninvasive, label-free, 3D optical coherence tomography (OCT) method to rapidly (2.5 min) image large sample volumes (1 mm3) to assess cell viability and distribution within scaffolds. OCT imaging was assessed using a model scaffold-cell system consisting of a polysaccharide-based hydrogel seeded with human Jurkat cells. Four test systems were used: hydrogel seeded with live cells, hydrogel seeded with heat-shocked or fixed dead cells and hydrogel without any cells. Time series OCT images demonstrated changes in the time-dependent speckle patterns due to refractive index (RI) variations within live cells that were not observed for pure hydrogel samples or hydrogels with dead cells. The changes in speckle patterns were used to generate live-cell contrast by image subtraction. In this way, objects with large changes in RI were binned as live cells. Using this approach, on average, OCT imaging measurements counted 326 ± 52 live cells per 0.288 mm3 for hydrogels that were seeded with 288 live cells (as determined by the acridine orange-propidium iodide cell counting method prior to seeding cells in gels). Considering the substantial uncertainties in fabricating the scaffold-cell constructs, such as the error from pipetting and counting cells, a 13% difference in the live-cell count is reasonable. Additionally, the 3D distribution of live cells was mapped within a hydrogel scaffold to assess the uniformity of their distribution across the volume. Our results demonstrate a real-time, noninvasive method to rapidly assess the spatial distribution of live cells within a 3D scaffold that could be useful for assessing tissue-engineered medical products.


