2023-05-15 エディンバラ大学
◆CoDE-ACSは、患者の心臓発作を迅速に切り捨てるだけでなく、高いトロポニンレベル(心臓発作後によく上昇する血液中のタンパク質)を心臓発作に起因するものと他の状態と区別するのにも医師の助けになる可能性があります。
◆エディンバラ大学の研究者によって開発されたこのAIツールは、年齢、性別、基礎疾患にかかわらず優れたパフォーマンスを発揮し、誤診断と人口の不平等を減らす可能性を示しています。
◆専門家は、CoDE-ACSが緊急医療をより効率的かつ効果的にする可能性があり、安全に帰宅できる患者を迅速に特定し、さらなる検査のために入院が必要な患者を医師に明示することができると述べています。
<関連情報>
- https://www.ed.ac.uk/news/2023/ai-tool-could-improve-heart-attack-diagnosis
- https://www.nature.com/articles/s41591-023-02325-4
心筋トロポニン濃度を用いた心筋梗塞の機械学習による診断法 Machine learning for diagnosis of myocardial infarction using cardiac troponin concentrations
Dimitrios Doudesis,Kuan Ken Lee,Jasper Boeddinghaus,Anda Bularga,Amy V. Ferry,Chris Tuck,Matthew T. H. Lowry,Pedro Lopez-Ayala,Thomas Nestelberger,Luca Koechlin,Miguel O. Bernabeu,Lis Neubeck,Atul Anand,Karen Schulz,Fred S. Apple,William Parsonage,Jaimi H. Greenslade,Louise Cullen,John W. Pickering,Martin P. Than,Alasdair Gray,Christian Mueller,Nicholas L. Mills & CoDE-ACS Investigators
Nature Medicine Published:11 May 2023
DOI:https://doi.org/10.1038/s41591-023-02325-4
Abstract
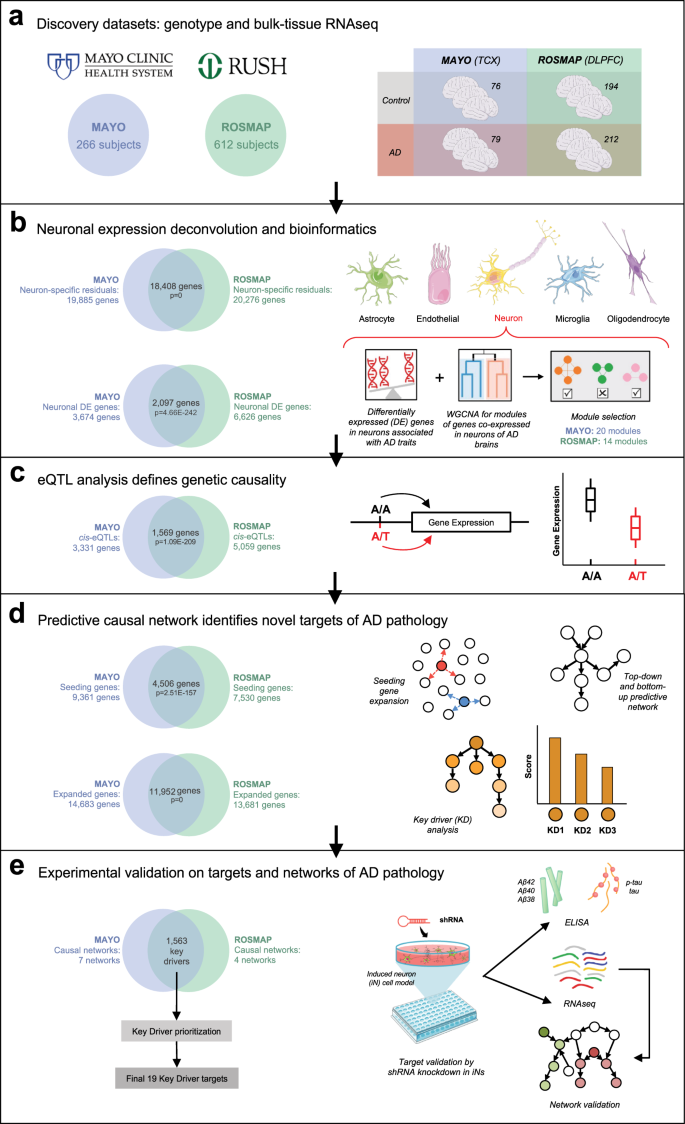
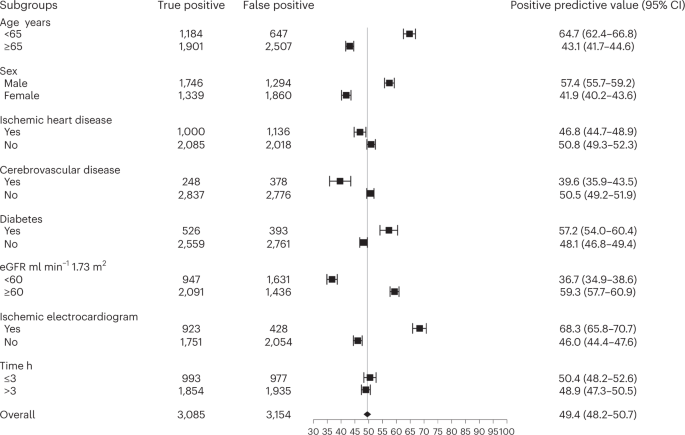
Although guidelines recommend fixed cardiac troponin thresholds for the diagnosis of myocardial infarction, troponin concentrations are influenced by age, sex, comorbidities and time from symptom onset. To improve diagnosis, we developed machine learning models that integrate cardiac troponin concentrations at presentation or on serial testing with clinical features and compute the Collaboration for the Diagnosis and Evaluation of Acute Coronary Syndrome (CoDE-ACS) score (0–100) that corresponds to an individual’s probability of myocardial infarction. The models were trained on data from 10,038 patients (48% women), and their performance was externally validated using data from 10,286 patients (35% women) from seven cohorts. CoDE-ACS had excellent discrimination for myocardial infarction (area under curve, 0.953; 95% confidence interval, 0.947–0.958), performed well across subgroups and identified more patients at presentation as low probability of having myocardial infarction than fixed cardiac troponin thresholds (61 versus 27%) with a similar negative predictive value and fewer as high probability of having myocardial infarction (10 versus 16%) with a greater positive predictive value. Patients identified as having a low probability of myocardial infarction had a lower rate of cardiac death than those with intermediate or high probability 30 days (0.1 versus 0.5 and 1.8%) and 1 year (0.3 versus 2.8 and 4.2%; P < 0.001 for both) from patient presentation. CoDE-ACS used as a clinical decision support system has the potential to reduce hospital admissions and have major benefits for patients and health care providers.