2023-11-27 タフツ大学
◆60のアルコール摂取に関連する代謝物を調査し、長期間にわたる適度なアルコール摂取がCVDリスクを増加させる循環代謝物と、その逆にCVDリスクを低下させる循環代謝物を特定しました。異なる種類のアルコールによって異なる代謝反応が引き起こされ、ビールの影響は全体的にワインや蒸留酒よりも弱いことが示されました。これにより、アルコールの心臓への影響を理解し、対象的な予防と治療につながるような研究が必要であることが強調されました。
<関連情報>
- https://now.tufts.edu/2023/11/27/alcohol-consumption-may-have-positive-and-negative-effects-cardiovascular-disease-risk
- https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-03149-2
循環代謝物がアルコール摂取と心血管疾患との関係を示すかもしれない Circulating metabolites may illustrate relationship of alcohol consumption with cardiovascular disease
Yi Li,Mengyao Wang,Xue Liu,Jian Rong,Patricia Emogene Miller,Roby Joehanes,Tianxiao Huan,Xiuqing Guo,Jerome I. Rotter,Jennifer A. Smith,Bing Yu,Matthew Nayor,Daniel Levy,Chunyu Liu & Jiantao Ma
BMC Medicine Published:16 November 2023
DO:Ihttps://doi.org/10.1186/s12916-023-03149-2
Abstract
Background
Metabolite signatures of long-term alcohol consumption are lacking. To better understand the molecular basis linking alcohol drinking and cardiovascular disease (CVD), we investigated circulating metabolites associated with long-term alcohol consumption and examined whether these metabolites were associated with incident CVD.
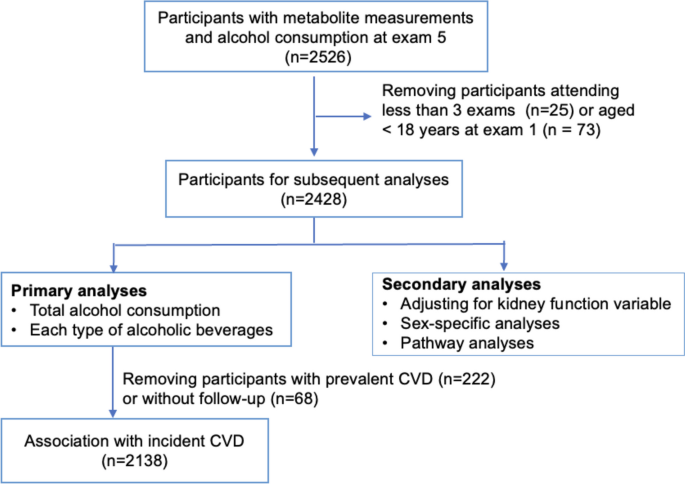
Methods
Cumulative average alcohol consumption (g/day) was derived from the total consumption of beer, wine, and liquor on average of 19 years in 2428 Framingham Heart Study Offspring participants (mean age 56 years, 52% women). We used linear mixed models to investigate the associations of alcohol consumption with 211 log-transformed plasma metabolites, adjusting for age, sex, batch, smoking, diet, physical activity, BMI, and familial relationship. Cox models were used to test the association of alcohol-related metabolite scores with fatal and nonfatal incident CVD (myocardial infarction, coronary heart disease, stroke, and heart failure).
Results
We identified 60 metabolites associated with cumulative average alcohol consumption (p < 0.05/211 ≈ 0.00024). For example, 1 g/day increase of alcohol consumption was associated with higher levels of cholesteryl esters (e.g., CE 16:1, beta = 0.023 ± 0.002, p = 6.3e - 45) and phosphatidylcholine (e.g., PC 32:1, beta = 0.021 ± 0.002, p = 3.1e - 38). Survival analysis identified that 10 alcohol-associated metabolites were also associated with a differential CVD risk after adjusting for age, sex, and batch. Further, we built two alcohol consumption weighted metabolite scores using these 10 metabolites and showed that, with adjustment age, sex, batch, and common CVD risk factors, the two scores had comparable but opposite associations with incident CVD, hazard ratio 1.11 (95% CI = [1.02, 1.21], p = 0.02) vs 0.88 (95% CI = [0.78, 0.98], p = 0.02).
Conclusions
We identified 60 long-term alcohol consumption-associated metabolites. The association analysis with incident CVD suggests a complex metabolic basis between alcohol consumption and CVD.
