2024-01-23 カリフォルニア大学サンディエゴ校(UCSD)
◆研究によれば、COMPOSERと呼ばれるAIアルゴリズムが17%の死亡率削減に貢献しました。このアルゴリズムは患者の150以上の変数を監視し、高い敗血症感染リスクを示す場合は看護スタッフに通知します。COMPOSERの導入前後で6,000人以上の患者入院を調査し、AIディープラーニングモデルを使用した初の研究であり、患者アウトカムの改善が報告されました。
<関連情報>
- https://today.ucsd.edu/story/study-ai-surveillance-tool-successfully-helps-to-predict-sepsis-saves-lives
- https://www.nature.com/articles/s41746-023-00986-6
ディープラーニングによる敗血症予測モデルがケアの質と生存に与える影響 Impact of a deep learning sepsis prediction model on quality of care and survival
Aaron Boussina, Supreeth P. Shashikumar, Atul Malhotra, Robert L. Owens, Robert El-Kareh, Christopher A. Longhurst, Kimberly Quintero, Allison Donahue, Theodore C. Chan, Shamim Nemati & Gabriel Wardi
npj Digital Medicine Published:23 January 2024
DOI:https://doi.org/10.1038/s41746-023-00986-6
Abstract
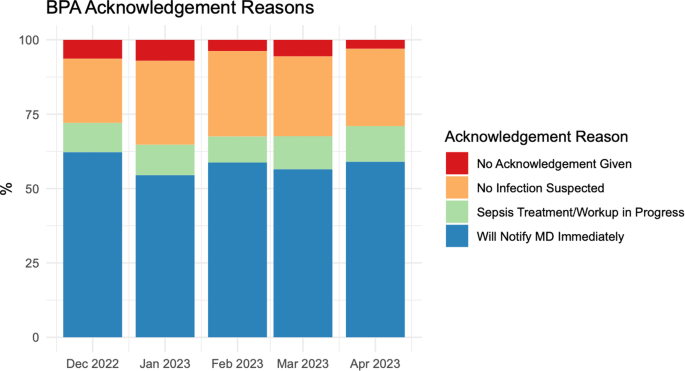
Sepsis remains a major cause of mortality and morbidity worldwide. Algorithms that assist with the early recognition of sepsis may improve outcomes, but relatively few studies have examined their impact on real-world patient outcomes. Our objective was to assess the impact of a deep-learning model (COMPOSER) for the early prediction of sepsis on patient outcomes. We completed a before-and-after quasi-experimental study at two distinct Emergency Departments (EDs) within the UC San Diego Health System. We included 6217 adult septic patients from 1/1/2021 through 4/30/2023. The exposure tested was a nurse-facing Best Practice Advisory (BPA) triggered by COMPOSER. In-hospital mortality, sepsis bundle compliance, 72-h change in sequential organ failure assessment (SOFA) score following sepsis onset, ICU-free days, and the number of ICU encounters were evaluated in the pre-intervention period (705 days) and the post-intervention period (145 days). The causal impact analysis was performed using a Bayesian structural time-series approach with confounder adjustments to assess the significance of the exposure at the 95% confidence level. The deployment of COMPOSER was significantly associated with a 1.9% absolute reduction (17% relative decrease) in in-hospital sepsis mortality (95% CI, 0.3%–3.5%), a 5.0% absolute increase (10% relative increase) in sepsis bundle compliance (95% CI, 2.4%–8.0%), and a 4% (95% CI, 1.1%–7.1%) reduction in 72-h SOFA change after sepsis onset in causal inference analysis. This study suggests that the deployment of COMPOSER for early prediction of sepsis was associated with a significant reduction in mortality and a significant increase in sepsis bundle compliance.


