2024-02-14 ミシガン大学
 Multidrug resistant bacteria inside a biofilm. Image credit: iStock
Multidrug resistant bacteria inside a biofilm. Image credit: iStock
<関連情報>
- https://news.umich.edu/widely-used-ai-tool-for-early-sepsis-detection-may-be-cribbing-doctors-suspicions/
- https://ai.nejm.org/doi/10.1056/AIoa2300032
治療開始前の敗血症予測モデルの評価 Evaluation of Sepsis Prediction Models before Onset of Treatment
Fahad Kamran, Ph.D.; Donna Tjandra, M.S. ; Andrew Heiler, M.B.A. ; Jessica Virzi, M.S.N. ; Karandeep Singh, M.D.; Jessie E. King, M.D., Ph.D.; Thomas S. Valley, M.D.; M.Sc. , and Jenna Wiens, Ph.D
NEJM AI Published February: 7, 2024
DOI: 10.1056/AIoa2300032
Abstract
BACKGROUND
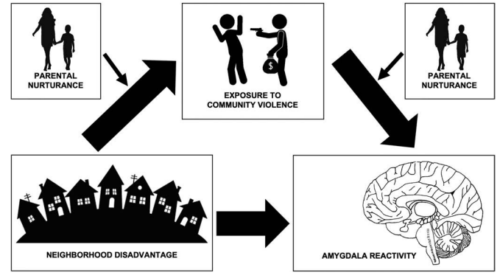
Timely interventions, such as antibiotics and intravenous fluids, have been associated with reduced mortality in patients with sepsis. Artificial intelligence (AI) models that accurately predict risk of sepsis onset could speed the delivery of these interventions. Although sepsis models generally aim to predict its onset, clinicians might recognize and treat sepsis before the sepsis definition is met. Predictions occurring after sepsis is clinically recognized (i.e., after treatment begins) may be of limited utility. Researchers have not previously investigated the accuracy of sepsis risk predictions that are made before treatment begins. Thus, we evaluate the discriminative performance of AI sepsis predictions made throughout a hospitalization relative to the time of treatment.
METHODS
We used a large retrospective inpatient cohort from the University of Michigan’s academic medical center (2018–2020) to evaluate the Epic sepsis model (ESM). The ability of the model to predict sepsis, both before sepsis criteria are met and before indications of treatment plans for sepsis, was evaluated in terms of the area under the receiver operating characteristic curve (AUROC). Indicators of a treatment plan were identified through electronic data capture and included the receipt of antibiotics, fluids, blood culture, and/or lactate measurement. The definition of sepsis was a composite of the Centers for Disease Control and Prevention’s surveillance criteria and the severe sepsis and septic shock management bundle definition.
RESULTS
The study included 77,582 hospitalizations. Sepsis occurred in 3766 hospitalizations (4.9%). ESM achieved an AUROC of 0.62 (95% confidence interval [CI], 0.61 to 0.63) when including predictions before sepsis criteria were met and in some cases, after clinical recognition. When excluding predictions after clinical recognition, the AUROC dropped to 0.47 (95% CI, 0.46 to 0.48).
CONCLUSIONS
We evaluate a sepsis risk prediction model to measure its ability to predict sepsis before clinical recognition. Our work has important implications for future work in model development and evaluation, with the goal of maximizing the clinical utility of these models. (Funded by Cisco Research and others.)