2024-05-21 カロリンスカ研究所(KI)
<関連情報>
- https://news.ki.se/inflammatory-bowel-disease-may-increase-risk-of-heart-failure
- https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehae338/7676429
炎症性腸疾患における心不全リスク:スウェーデンの集団ベース研究 Risk of heart failure in inflammatory bowel disease: a Swedish population-based study
Jiangwei Sun, PhD, Jialu Yao, MSc, Ola Olén, MD, PhD, Jonas Halfvarson, MD, PhD, David Bergman, MD, PhD, Fahim Ebrahimi, MD, MSc, Annika Rosengren, MD, PhD, Johan Sundström, MD, PhD, Jonas F Ludvigsson, MD, PhD
European Heart Journal Published:21 May 2024
DOI:https://doi.org/10.1093/eurheartj/ehae338
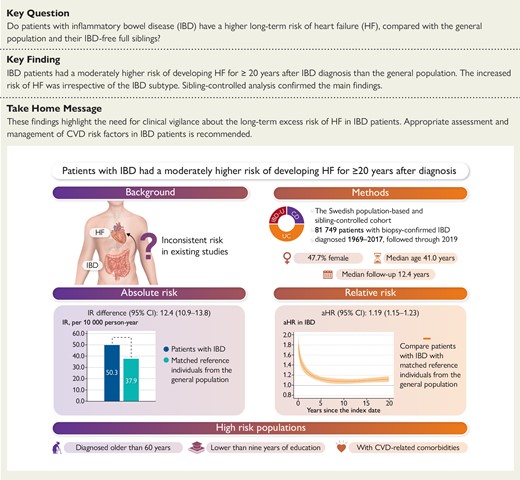
Graphical Abstract
Abstract
Background and Aims
Dysregulation of inflammatory and immune responses has been implicated in the pathogenesis of heart failure (HF). But even if inflammation is a prerequisite for inflammatory bowel disease (IBD), little is known about HF risk in IBD.
Methods
In this Swedish nationwide cohort, patients with biopsy-confirmed IBD were identified between 1969 and 2017 [n = 81,749, Crohn’s disease (CD, n = 24,303), ulcerative colitis (UC, n = 45,709), and IBD-unclassified (IBD-U, n = 11,737)]. Each patient was matched with up to five general population reference individuals (n = 382,190) and IBD-free full siblings (n = 95,239) and followed until 31 December 2019. Flexible parametric survival models estimated the adjusted hazard ratio (aHR) and standardized cumulative incidence for HF, with 95% confidence intervals (CI).
Results
There were 5,582 incident HF identified in IBD patients (incidence rate [IR]: 50.3/10,000 person-years) and 20,343 in reference individuals (IR: 37.9) during a median follow-up of 12.4 years. IBD patients had a higher risk of HF than reference individuals (aHR 1.19, 95% CI 1.15 to 1.23). This increased risk remained significant ≥20 years after IBD diagnosis, leading to one extra HF case per 130 IBD patients until then. The increased risk was also observed across IBD subtypes: CD (IR: 46.9 vs. 34.4; aHR 1.28 [1.20 to 1.36]), UC (IR: 50.1 vs. 39.7; aHR 1.14 [1.09 to 1.19]), and IBD-U (IR: 60.9 vs. 39.0; aHR 1.28 [1.16 to 1.42]). Sibling-controlled analyses showed slightly attenuated association (IBD: aHR 1.10 [1.03 to 1.19]).
Conclusions
Patients with IBD had a moderately higher risk of developing HF for ≥20 years after IBD diagnosis than the general population.