2024-06-07 エディンバラ大学
英国では、毎年10万人の女性のうち12人が妊娠関連の死を経験し、特に少数民族や社会的に困窮している地域の女性に多いです。さらに、妊娠中や出産後に重篤な病気を発症する女性は70~90人にのぼります。これは、長期的な健康問題を抱える女性の妊娠や高齢妊婦の増加に伴い、深刻な問題となっています。
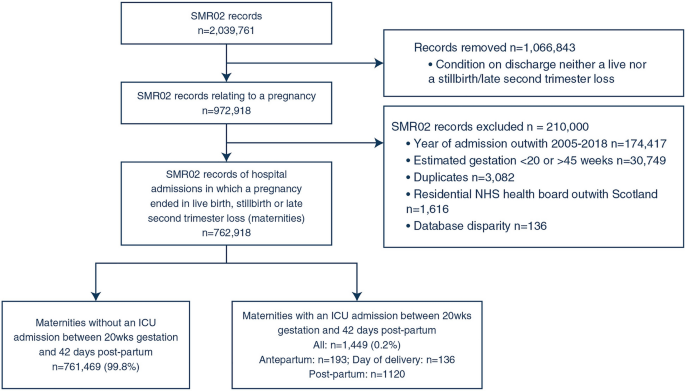
◆エディンバラ大学の研究者たちは、2005年から2018年までのスコットランドの病院での76万件以上の出産データを解析しました。その結果、約1,500人の女性が集中治療室に入院し、その主な理由は産後出血でした。集中治療室に入院した女性は、入院しなかった女性と比べて死亡リスクが40倍高く、特に心血管疾患が原因でした。また、集中治療室に入院した女性の赤ちゃんは、退院後に高度な医療を必要とする確率が13倍高いことが分かりました。
◆研究者たちは、集中治療から退院した女性の4分の1が1年以内に再入院しており、産後ケアは集中治療の専門家と産科専門家が連携して行うべきだと強調しています。この研究は「Intensive Care Medicine」誌に掲載されました。
<関連情報>
- https://www.ed.ac.uk/news/2024/maternal-care-insights-point-to-risks-of-critical
- https://link.springer.com/article/10.1007/s00134-024-07417-4
妊産婦の重症入院が短期および長期の妊産婦転帰と出産転帰に及ぼす影響の測定 Measuring the impact of maternal critical care admission on short- and longer-term maternal and birth outcomes
John A. Masterson,Imad Adamestam,Monika Beatty,James P. Boardman,Louis Chislett,Pamela Johnston,Judith Joss,Heather Lawrence,Kerry Litchfield,Nicholas Plummer,Stella Rhode,Timothy Walsh,Arlene Wise,Rachael Wood,Christopher J. Weir & Nazir I. Lone
Intensive Care Medicine Published:07 June 2024
DOI:https://doi.org/10.1007/s00134-024-07417-4
Abstract
Purpose
Factors increasing the risk of maternal critical illness are rising in prevalence in maternity populations. Studies of general critical care populations highlight that severe illness is associated with longer-term physical and psychological morbidity. We aimed to compare short- and longer-term outcomes between women who required critical care admission during pregnancy/puerperium and those who did not.
Methods
This is a cohort study including all women delivering in Scottish hospitals between 01/01/2005 and 31/12/2018, using national healthcare databases. The primary exposure was intensive care unit (ICU) admission, while secondary exposures included high dependency unit admission. Outcomes included hospital readmission (1-year post-hospital discharge, 1-year mortality, psychiatric hospital admission, stillbirth, and neonatal critical care admission). Multivariable Cox and logistic regression were used to report hazard ratios (HR) and odds ratios (OR) of association between ICU admission and outcomes.
Results
Of 762,918 deliveries, 1449 (0.18%) women were admitted to ICU, most commonly due to post-partum hemorrhage (225, 15.5%) followed by eclampsia/pre-eclampsia (133, 9.2%). Over-half (53.8%) required mechanical ventilation. One-year hospital readmission was more frequent in women admitted to ICU compared with non-ICU populations [24.5% (n = 299) vs 8.9% (n = 68,029)]. This association persisted after confounder adjustment (HR 1.93, 95% confidence interval [CI] 1.33, 2.81, p < 0.001). Furthermore, maternal ICU admission was associated with increased 1-year mortality (HR 40.06, 95% CI 24.04, 66.76, p < 0.001), stillbirth (OR 12.31, 95% CI 7.95,19.08, p < 0.001) and neonatal critical care admission (OR 6.99, 95% CI 5.64,8.67, p < 0.001) after confounder adjustment.
Conclusion
Critical care admission increases the risk of adverse short-term and long-term maternal, pregnancy and neonatal outcomes. Optimizing long-term post-partum care may benefit maternal critical illness survivors.