2024-10-23 バッファロー大学(UB)
<関連情報>
- https://www.buffalo.edu/news/releases/2024/10/UB-neurology-study-severe-multiple-sclerosis-.html
- https://academic.oup.com/braincomms/article/6/4/fcae226/7702529
- https://link.springer.com/article/10.1007/s00415-024-12420-2
- https://www.msard-journal.com/article/S2211-0348(24)00207-4/abstract
重症進行性多発性硬化症における認知機能 Cognitive function in severe progressive multiple sclerosis
Dejan Jakimovski, Robert Zivadinov, Zachary Weinstock, Alex Burnham, Taylor R Wicks, Christopher Suchan, Tommaso Sciortino, Ferdinand Schweser, Niels Bergsland, Michael G Dwyer …
Brain Communications Published:02 July 2024
DOI:https://doi.org/10.1093/braincomms/fcae226
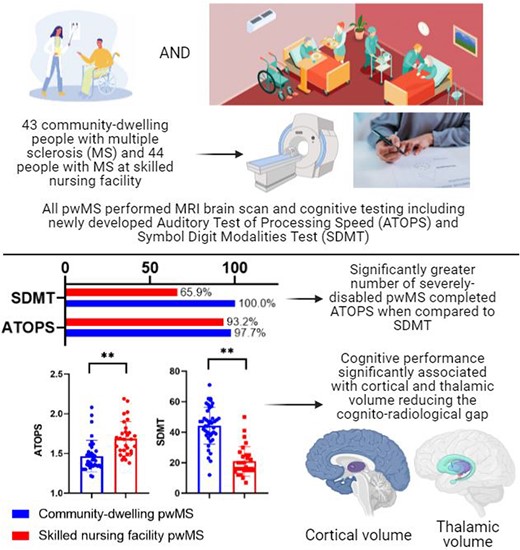
Graphical Abstract
Abstract
Cognitive impairment is common in multiple sclerosis and negatively impacts quality of life. Cognitive status has yet to be described in people with severe progressive multiple sclerosis, in whom conventional neuropsychological testing is exceptionally difficult. The objective for the study was to characterize cognitive performance in severe progressive multiple sclerosis and compare them with age-, sex- and disease duration-matched less disabled people with multiple sclerosis using a specifically developed auditory, non-motor test of attention/cognitive processing speed—Auditory Test of Processing Speed. Also, we aimed to determine the relationship between cognitive performance and MRI-based outcomes in these matched cohorts. The Comprehensive Assessment of Severely Affected Multiple Sclerosis study was carried out at the University at Buffalo and the Boston Home, a skilled nursing facility in Dorchester, MA. Inclusion criteria were age 30–80 years and expanded disability status scale 3.0–6.5 for community-dwelling and 7.0–9.5 for skilled nursing facility people with multiple sclerosis. The cognitive assessment was performed using the Brief International Cognitive Assessment for Multiple Sclerosis consisting of Symbol Digit Modalities Test, Brief Visuospatial Memory Test—Revised, California Verbal Learning Test—2nd edition along with Auditory Test of Processing Speed, Paced Auditory Serial Addition Test—3 second and Controlled Oral Word Association Test. MRI scans were retrospectively collected and analysed for lesion and volumetric brain measurements. The rate of completion and performance of the cognitive tests was compared between the groups, and the relationship with MRI measures was determined using sex, age and years of education-adjusted linear regression models. Significantly greater percentage of the severe multiple sclerosis group completed Auditory Test of Processing Speed when compared with the current gold standard of Symbol Digit Modalities Test (93.2% versus 65.9%). Severe progressive multiple sclerosis had worse cognitive performance in all cognitive domains with greatest differences for cognitive processing speed (Symbol Digit Modalities Test > Paced Auditory Serial Addition Test—3 second > Auditory Test of Processing Speed, Cohen’s d < 2.13, P < 0.001), learning and memory (Cohen’s d < 1.1, P < 0.001) and language (Controlled Oral Word Association Test with Cohen’s d = 0.97, P < 0.001). Multiple cognitive domains were significantly associated with lower thalamic (standardized β < 0.419, P < 0.006) and cortical (standardized β < 0.26, P < 0.031) volumes. Specially designed (auditory) cognitive processing speed tests may provide more sensitive screening of cognitive function in severe progressive multiple sclerosis. The cognitive profile of severe multiple sclerosis is proportional to their physical outcomes and best explained by decreased grey matter volume.
施設入所中の重症多発性硬化症患者の神経画像評価から、皮質灰白質病理の重要な役割が明らかになった:CASA-MS症例対照研究の結果 Neuroimaging assessment of facility-bound severely-affected MS reveals the critical role of cortical gray matter pathology: results from the CASA–MS case-controlled study
Robert Zivadinov,Dejan Jakimovski,Alex Burnham,Jens Kuhle,Zachary Weinstock,Taylor R. Wicks,Murali Ramanathan,Tommaso Sciortino,Mark Ostrem,Christopher Suchan,Michael G. Dwyer,Jessica Reilly,Niels Bergsland,Ferdinand Schweser,Cheryl Kennedy,David Young-Hong,Svetlana Eckert,David Hojnacki,Ralph H. B. Benedict & Bianca Weinstock-Guttman
Journal of Neurology Published:17 May 2024
DOI:https://doi.org/10.1007/s00415-024-12420-2
Abstract
Background
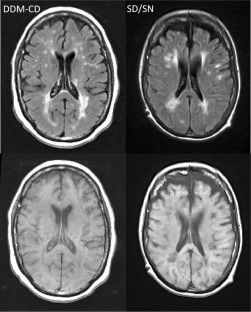
A subgroup of people with multiple sclerosis (pwMS) will develop severe disability. The pathophysiology underlying severe MS is unknown. The comprehensive assessment of severely affected MS (CASA–MS) was a case-controlled study that compared severely disabled in skilled nursing (SD/SN) (EDSS ≥ 7.0) to less-disabled (EDSS 3.0–6.5) community dwelling (CD) progressive pwMS, matched on age-, sex- and disease-duration (DDM).
Objectives
To identify neuroimaging and molecular biomarker characteristics that distinguish SD/SN from DDM–CD progressive pwMS.
Methods
This study was carried at SN facility and at a tertiary MS center. The study collected clinical, molecular (serum neurofilament light chain, sNfL and glial acidic fibrillary protein, sGFAP) and MRI quantitative lesion-, brain volume-, and tissue integrity-derived measures. Statistical analyses were controlled for multiple comparisons.
Results
42 SD/SN and 42 DDM–CD were enrolled. SD/SN pwMS showed significantly lower cortical volume (CV) (p < 0.001, d = 1.375) and thalamic volume (p < 0.001, d = 0.972) compared to DDM–CD pwMS. In a logistic stepwise regression model, the SD/SN pwMS were best differentiated from the DDM–CD pwMS by lower CV (p < 0.001) as the only significant predictor, with the accuracy of 82.3%. No significant differences between the two groups were observed for medulla oblongata volume, a proxy for spinal cord atrophy and white matter lesion burden, while there was a statistical trend for numerically higher sGFAP in SD/SN pwMS.
Conclusions
The CASA–MS study showed significantly more gray matter atrophy in severe compared to less-severe progressive MS.
重度多発性硬化症患者における動的障害測定は臨床的・放射線学的ギャップを減少させる Dynamic disability measures decrease the clinico-radiological gap in people with severely affected multiple sclerosis
Dejan Jakimovsk∙ Bianca Weinstock-Guttman∙ Alex Burnham∙ … ∙ David Hojnacki∙ Ralph HB Benedict∙ Robert Zivadinov
Multiple Sclerosis Published:April 22, 2024
DOI:https://doi.org/10.1016/j.msard.2024.105630
Highlights
•Expanded disability status scale (EDSS) is limited when utilized in highly disabled people with multiple sclerosis (pwMS).
•This study explores the utility of multiple disability MS scales for assessment of severely affected pwMS.
•The scripps neurological rating scale (SNRS) and combinatorial weight-adjusted disability score (CombiWISE) provide dynamic and greater spread of scores for disability assessment.
•SNRS and CombiWISE significantly reduce the clinic-radiological gap in severely-affected pwMS.
Abstract
Background
Expanded Disability Status Scale (EDSS) is limited when utilized in highly disabled people with multiple sclerosis (pwMS).
Objetive
To explore the relationship between disability measures and MRI outcomes in severely-affected pwMS.
Methods
PwMS recruited from The Boston Home (TBH), a specialized residential facility for severly-affected pwMS and University at Buffalo (UB) MS Center were assessed using EDSS, MS Severity Scale, age-related MSS, Scripps Neurological Rating Scale (SNRS) and Combinatorial Weight-Adjusted Disability Score (CombiWISE). In all scores except SNRS, higher score indicates greater disability. MRI measures of T1, T2-lesion volume (LV), whole brain, gray matter, medulla oblongata and thalamic volumes (WBV, GMV, MOV, TV) and thalamic dysconnectivity were obtained.
Results
Greatest disability differences between the TBH and UB pwMS were in SNRS (24.4 vs 71.9, p < 0.001, Cohen’s d = 4.05) and CombiWISE (82.3 vs. 38.9, p < 0.001, Cohen’s d = 4.02). In combined analysis of all pwMS, worse SNRS scores were correlated with worse MRI pathology in 8 out of 9 outcomes. EDSS only with 3 measures (GMV, MOV and TV). In severely-affected pwMS, SNRS was associated with T1-LV, T2-LV and WBV (not surviving false discovery rate (FDR) correction for multiple comparisons) whereas EDSS did not.
Conclusion
Granular and dynamic disability measures may bridge the clinico-radiologcal gap present in severely affected pwMS.


