2025-03-11 東京科学大学
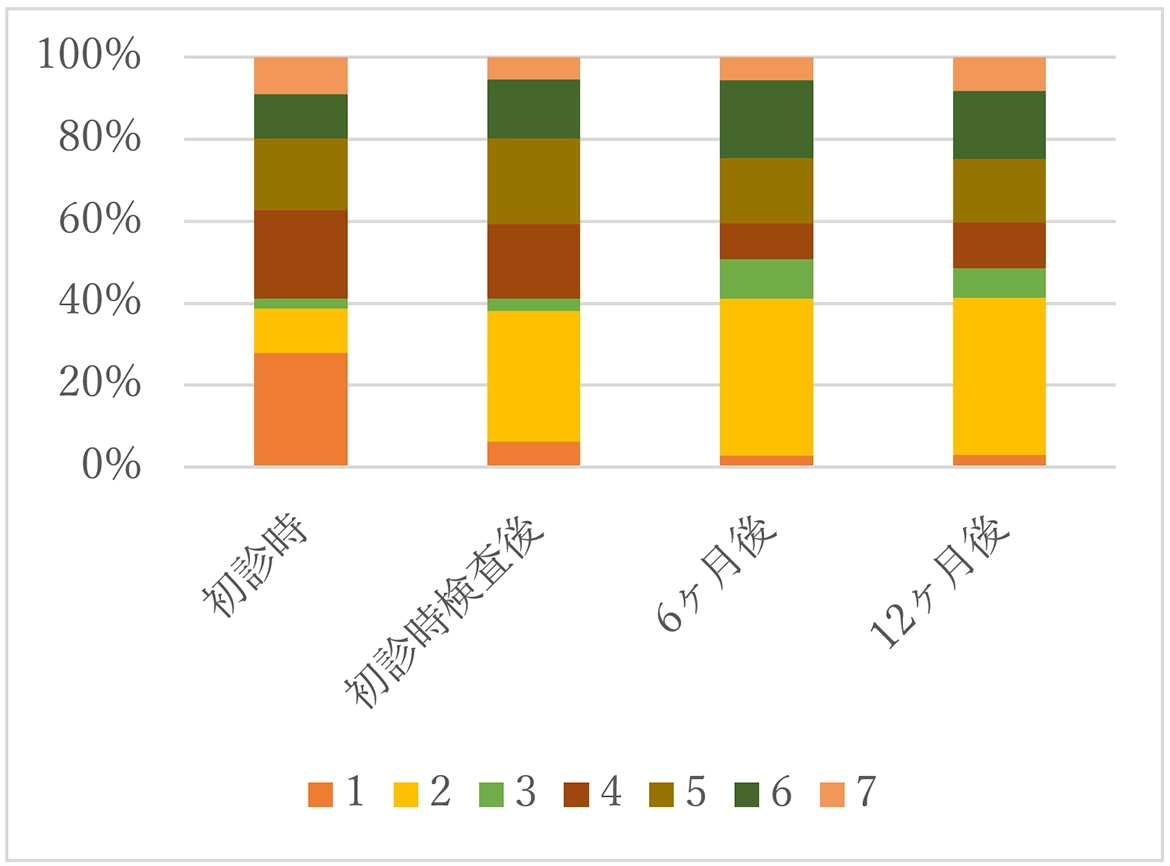
図1.経口摂取状況の変化。
<関連情報>
- https://www.isct.ac.jp/ja/news/2jg4xf6r7mdl
- https://www.thejpd.org/article/S0022-3913(25)00094-0/abstract
訪問歯科診療を通じた地域居住の介護依存症患者における嚥下障害の進行と関連因子 12ヵ月間のレトロスペクティブ・コホート研究 Dysphagia progression and related factors in community-dwelling care-dependent patients through home-visit dental care: A 12-month retrospective cohort study
Kohei Yamaguchi, DDS, PhD∙ Sayaka Komori, DDS∙ Ryosuke Yanagida, DDS, PhD∙ … ∙ Kanako Yoshimi, DDS, PhD∙ Kazuharu Nakagawa, DDS, PhD∙ Haruka Tohara, DDS, PhD
The Journal of Prosthetic Dentistry Published:March 8, 2025
DOI:https://doi.org/10.1016/j.prosdent.2025.02.006
Abstract
Statement of problem
Reports on the progress and characteristics of patients with dysphagia who require professional care at home or in a nursing home are sparse.
Purpose
The purpose of this 12-month retrospective cohort study was to investigate the characteristics of care-dependent patients with dysphagia in the community and the factors related to oral intake scale outcomes over 12 months of dysphagia rehabilitation through home-visit dental care.
Material and methods
A total of 323 participants receiving care at home or in a nursing facility who underwent dysphagia rehabilitation through home-visit dental care were enrolled. The outcome was the Functional Oral Intake Scale (FOIS) score at baseline and after 6 and 12 months of rehabilitation. Multivariable linear regression analysis was used to explore the factors associated with FOIS scores before and after dysphagia rehabilitation (α=.05).
Results
Approximately 90% of the participants had maintained or improved FOIS scores after 12 months. A difference in associated factors was observed between FOIS scores at baseline and after rehabilitation. Aspiration pneumonia history (B=-1.040, P<.001) and residential environment (B=-0.489, P=.035) were significantly linked to baseline FOIS scores but were not significant predictors of FOIS scores after 6 months (P>.05).
Conclusions
The findings demonstrate that FOIS scores improved in the community with 12-month dysphagia rehabilitation, although the rehabilitation was affected by the overall condition. This underscores the importance of accessible and tailored community-based services for those dependent on care services.