2025-04-16 ラトガース大学
<関連情報>
- https://www.rutgers.edu/news/frequent-use-antibiotics-infants-and-young-children-may-increase-risk-asthma-allergies-and
- https://academic.oup.com/jid/advance-article-abstract/doi/10.1093/infdis/jiaf191/8114163
- https://www.journalofinfection.com/article/S0163-4453(22)00004-4/fulltext
幼児期の抗生物質と小児慢性疾患:レトロスペクティブ・コホート研究 Early childhood antibiotics and chronic pediatric conditions: a retrospective cohort study
Matthew A Beier, MD, MFE , Soko Setoguchi, MD, DrPH , Tobias Gerhard, BSPharm, PhD , Jason Roy, PhD , Dawn Koffman, MS , Dinesh Mendhe, MS , Joanna Madej, MD , Brian L Strom, MD, MPH , Martin J Blaser, MD , Daniel B Horton, MD, MSCE
The Journal of Infectious Diseases Published:16 April 2025
DOI:https://doi.org/10.1093/infdis/jiaf191
Abstract
Background
Early-childhood antibiotic exposure has been implicated in the development of chronic pediatric conditions, but many studies leave concerns about unmeasured confounding. We evaluated associations between early-childhood antibiotic exposure and allergic, autoimmune, or neurodevelopmental/psychiatric conditions.
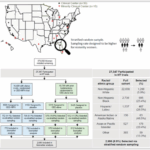
Methods
We performed a retrospective cohort study using electronic health records data from the United Kingdom (1987-2020). The primary exposure was antibiotic prescriptions between birth and age 2 years. Outcomes were diagnoses of chronic pediatric conditions (asthma/allergic, autoimmune, and neurodevelopmental/psychiatric) or forearm fracture (negative control). Adjusted hazard ratios with 95% confidence intervals were estimated using multivariable Cox regression models adjusted for maternal, child, and area-based socioeconomic status. A sibling-matched analysis was conducted using conditional Cox regression.
Results
Among 1,091,449 children, antibiotic exposure before age 2 was positively associated with asthma (hazard ratio 1.24, 1.22-1.26), food allergy (hazard ratio 1.33, 1.26-1.40), and allergic rhinitis (hazard ratio 1.06, 1.03-1.10), with stronger associations observed following multiple antibiotic courses. Findings from sibling-matched analyses were similar. Early-childhood antibiotic exposure was also dose-dependently associated with intellectual disability (5+ vs. 1-2 courses: hazard ratio 1.73, 1.49-2.01; sibling-matched: 2.79, 1.87-4.18), but not with celiac disease, inflammatory bowel disease, juvenile idiopathic arthritis, psoriasis, type 1 diabetes, attention-deficit/hyperactivity disorder, autism spectrum disorders, or anxiety. Sibling-matched results and a negative control outcome suggested minimal confounding bias.
Conclusions
Children receiving multiple antibiotic courses between birth and age 2 were more likely to develop asthma, food allergies, allergic rhinitis, and intellectual disability. However, risks of most autoimmune, neurodevelopmental, and psychiatric conditions studied were minimal following early-childhood antibiotic exposure.
抗生物質への曝露と小児における長期的な健康上の有害転帰: システマティックレビューとメタアナリシス Antibiotic exposure and adverse long-term health outcomes in children: A systematic review and meta-analysis
Quynh A Duong ∙ Laure F Pittet ∙ Nigel Curtis ∙ Petra Zimmermann
Journal of Infection Published:January 9, 2022
DOI:https://doi.org/10.1016/j.jinf.2022.01.005

Summary
Background
Antibiotics are amongst the most commonly used drugs in children. In addition to inducing antibiotic resistance, antibiotic exposure has been associated with adverse long-term health outcomes.
Methods
A systematic search using PRISMA guidelines to identify original studies reporting associations between antibiotic exposure and adverse long-term health outcomes in children. Overall pooled estimates of the odds ratios (ORs) were obtained using random-effects models.
Results
We identified 160 observational studies investigating 21 outcomes in 22,103,129 children. Antibiotic exposure was associated with an increased risk of atopic dermatitis (OR 1.40, 95% confidence interval (CI) 1.30–1.52, p < 0.01), allergic symptoms (OR 1.93, 95%CI 1.66–2.26, p < 0.01), food allergies (OR 1.35, 95%CI 1.20–1.52, p < 0.01), allergic rhinoconjunctivitis (OR 1.66, 95%CI 1.51–1.83, p < 0.01), wheezing (OR 1.81, 95%CI 1.65–1.97, p < 0.01), asthma (OR 1.96, 95%CI 1.76–2.17, p < 0.01), increased weight gain or overweight (OR 1.18, 95%CI 1.11–1.26, p < 0.01), obesity (OR 1.21, 95%CI 1.05–1.40, p < 0.01), juvenile idiopathic arthritis (OR 1.74, 95%CI 1.21–2.52, p < 0.01), psoriasis (OR 1.75, 95%CI 1.44–2.11, p < 0.01), autism spectrum disorders (OR 1.19, 95%CI 1.04–1.36, p = 0.01) and neurodevelopment disorders (OR 1.29, 95%CI 1.09–1.53, p < 0.01). Dose-response effects and stronger effects with broad-spectrum antibiotic were often reported. Antibiotic exposure was not associated with an altered risk of allergic sensitisation, infantile colic, abdominal pain, inflammatory bowel disease, celiac disease, type 1 diabetes, fluorosis, and attention deficit hyperactivity disorder.
Conclusion
Although a causal association cannot be determined from these studies, the results support the meticulous application of sound antibiotic stewardship to avoid potential adverse long-term health outcomes.