2025-05-26 北海道大学病院,国立がん研究センター,慶応義塾大学
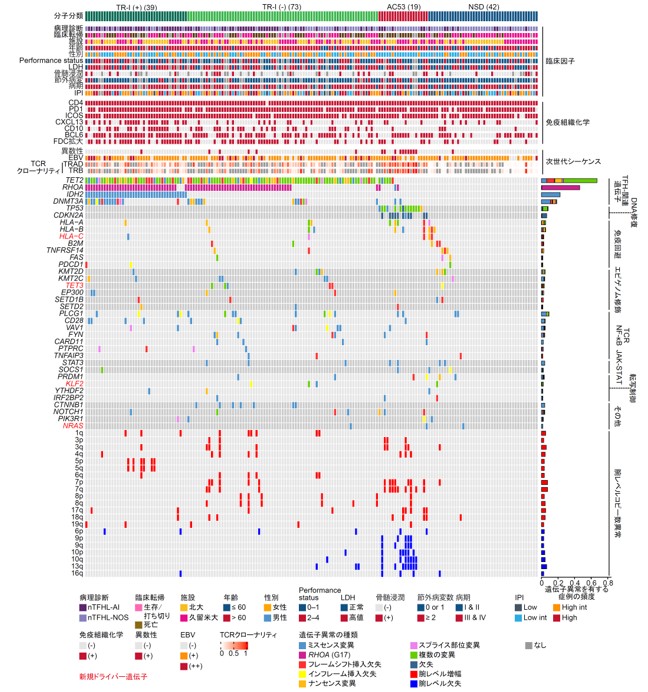
図1 nTFHL173例における遺伝子異常の全体像
<関連情報>
- https://www.ncc.go.jp/jp/information/researchtopics/2025/0526/index.html
- https://www.ncc.go.jp/jp/information/researchtopics/2025/0526/20250526.pdf
- https://www.nature.com/articles/s41375-025-02631-5
結節性T濾胞性ヘルパー細胞リンパ腫患者におけるTP53およびCDKN2Aの変化は予後不良サブグループを規定する TP53 and CDKN2A alterations define a poor prognostic subgroup in patients with nodal T follicular helper cell lymphoma
Yuta Ito,Joji Shimono,Keisuke Kawamoto,Kanako C. Hatanaka,Yasunori Kogure,Mariko Tabata,Yuki Saito,Kota Mizuno,Sara Horie,Yosuke Mizukami,Junji Koya,Koichi Murakami,Takanori Teshima,Yutaka Hatanaka,Kenichi Chiba,Ai Okada,Yuichi Shiraishi,Hiroaki Miyoshi,Yoshihiro Matsuno,Koichi Ohshima,Keisuke Kataoka & Masao Nakagawa
Leukemia Published:02 May 2025
DOI:https://doi.org/10.1038/s41375-025-02631-5
Abstract
Nodal T follicular helper cell lymphoma (nTFHL) exhibits unique immunophenotypes and somatic alterations, while the prognostic value of these alterations remains unclear. By analyzing 173 nTFHL cases, we identified 36 driver genes, including 4 novel ones (TET3, HLA-C, NRAS, and KLF2). Then, we classified nTFHL cases into four molecular subgroups by major driver alterations. TR-I (+) and TR-I (-) were characterized by TET2 and/or RHOA mutations with and without IDH2 mutations; AC53 by TP53 and/or CDKN2A alterations and aneuploidy; and NSD with no subgroup-defining alterations (namely without any of the above alterations). AC53 exhibited the worst survival, while NSD, particularly those lacking driver alterations, showed the best prognosis. nTFHL had a better prognosis than peripheral T-cell lymphoma, not otherwise specified, when TP53 and/or CDKN2A alterations were absent. Multivariable analyses showed that AC53, the presence of driver alterations, and international prognostic index high-risk were independently associated with worse survival. Finally, we developed a simple prognostic index (mTFHL-PI), which classified patients into three risk categories with a median OS of 181, 67, and 20 months, respectively. Our study identifies novel prognostic factors, namely TP53 and/or CDKN2A alterations and the presence of driver alterations, demonstrating the clinical relevance of molecular classification in nTFHL.