2025-05-26 国立循環器病研究センター
<関連情報>
- https://www.ncvc.go.jp/pr/release/pr_47247/
- https://jnnp.bmj.com/content/early/2025/04/24/jnnp-2024-335110
腎機能障害患者における脳卒中再発リスクの増加:MICON国際共同研究による個々の患者データのプール解析結果 Increased risk of recurrent stroke in patients with impaired kidney function: results of a pooled analysis of individual patient data from the MICON international collaboration
Jeremy Molad, Kaori Miwa, Philip S. Nash, Gareth Ambler, Jonathan Best, Duncan Wilson, Hen Hallevi, Simon Fandler-Höfler, Sebastian Eppinger, Houwei Du, Rustam Al-Shahi Salman, Rolf Jager, Gregory Y.H. Lip, Martina B. Goeldlin, Morin Beyeler, Philipp Bücke, Marwan El-Koussy, Heinrich Mattle, Leonidas D. Panos, Dianne H.K. van Dam-Nolen, Florian Dubost, Jeroen Hendrikse, Eline M. Kooi, Werner Mess, Paul J. Nederkoorn, Masayuki Shiozawa, Nicolas Christ, Maximilian Bellut, Sarah Gunkel, Chris Karayiannis, John Van Ly, Shaloo Singhal, Lee-Anne Slater, Young-Dae Kim, Tae-Jin Song, Keon-Joo Lee, Jae-Sung Lim, Hideo Hara, Masashi Nishihara, Jun Tanaka, Masaaki Yoshikawa, Derya S. Demirelli, Zeynep Tanriverdi, Ender Uysal, Shelagh B. Coutts, Francesca Chappell, Stephen Makin, Henry Mak, Kay-Cheong Teo, Debbie Y.K. Wong, Lisa Hert, Marta Kubacka, Philippe Lyrer, Alexandros Polymeris, Benjamin Wagner, Annaelle Zietz, Jill Abrigo, Cyrus Cheng, Winnie Chu, Thomas W.H. Leung, Suk F. Tsang, Brian Yiu, David Seiffge, Urs Fischer, Simon Jung, Christian Enzinger, Thomas Gattringer, Daniel Bos, Kazunori Toyoda, Felix Fluri, Thanh Phan, Velandai Srikanth, Ji-Hoe Heo, Hee-Joon Bae, Yusuke Yakushiji, Dilek N. Orken, Eric E. Smith, Joanna M. Wardlaw, Gary K.K. Lau, Stefan T. Engelter, Nils Peters, Yannie Soo, David C. Wheeler, Rob J. Simister, Natan M. Bornstein, David J. Werring, Einor Ben Assayag and Masatoshi Koga
Journal of Neurology, Neurosurgery & Psychiatry published: April 24, 2025
DOI:10.1136/jnnp-2024-335110
Abstract
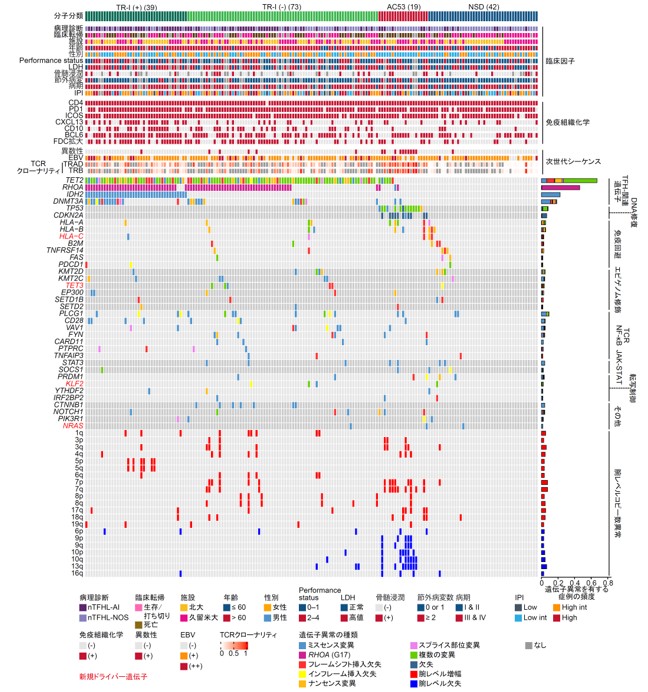
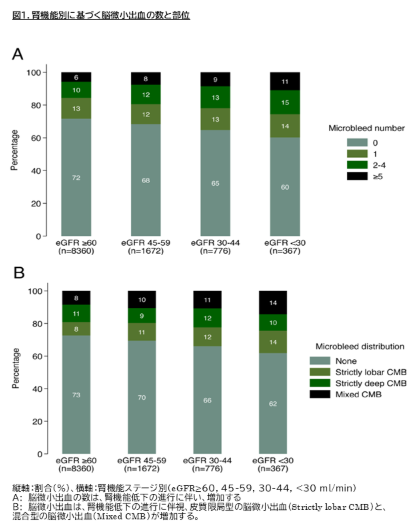
Background Patients with chronic kidney disease are at increased risk of stroke and frequently have cerebral microbleeds. Whether such patients also encounter an increased risk of recurrent stroke has not been firmly established. We aimed to determine whether impaired kidney function is associated with the risk of recurrent stroke, and microbleed presence, distribution and severity.
Methods We used pooled data from the Microbleeds International Collaborate Network to investigate associations of impaired kidney function, defined as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2. Our primary outcome was a composite of recurrent ischaemic stroke (IS) and intracranial haemorrhage (ICrH). Secondary outcomes included: (1) individual components of the primary outcome; (2) modification of the primary outcome by microbleed presence or anticoagulant use and (3) microbleed presence, distribution and severity.
Results 11 175 patients (mean age 70.7±12.6, 42% female) were included, of which 2815 (25.2%) had impaired kidney function. Compared with eGFR ≥60, eGFR <60 was associated with a higher risk of the primary outcome (adjusted HR, aHR 1.33 (95% CI 1.14 to 1.56), p<0.001) and higher rates of the recurrent IS (aHR 1.33 (95% CI 1.12 to 1.58)). Reduced eGFR was not associated with ICrH risk (aHR 1.07 (95% CI 0.70 to 1.60)). eGFR was also associated with microbleed presence (adjusted OR, aOR 1.14 (95% CI 1.03 to 1.26)) and severity (aOR 1.17 (95% CI 1.06 to 1.29)). Compared with having no microbleeds, eGFR was lower in those with strictly lobar microbleeds (adjusted mean difference (aMD) -2.10 mL/min/1.73 cm2 (95% CI -3.39 to -0.81)) and mixed microbleeds (aMD -2.42 (95% CI -3.70 to -1.15)), but not strictly deep microbleeds (aMD -0.67 (95% CI -1.85 to 0.51)).
Conclusions In patients with IS or transient ischaemic attack, impaired kidney function was associated with a higher risk of recurrent stroke and higher microbleeds burden, compared with those with normal kidney function. Further research is needed to investigate potential additional measures for secondary prevention in this high-risk group.