2025-06-11 カロリンスカ研究所(KI)
スウェーデン・カロリンスカ研究所の全国コホート研究(1974~2001年生まれ約130万人)で、児童期に暴力や親の精神疾患、薬物乱用、経済困難など逆境体験(ACE)を持つ女性は、子宮内膜症を発症するリスクが高いことが示されました。ACEが1つあるだけでも発症リスクが約20%増加し、5つ以上では最大60%増。特に暴力経験はリスクを2倍にするという強い関連が明らかにされました。
研究は国の登録データを用いた観察研究であり、因果関係の断定はできませんが、児童期ストレスが免疫機能の低下あるいは痛覚過敏を招く可能性が示唆されています。研究者は、ACE歴を踏まえた予防策や患者ケアの改善が必要と述べ、トラウマを考慮した包括的医療への重要性を強調しています。
<関連情報>
- https://news.ki.se/difficult-childhood-experiences-may-increase-the-risk-of-endometriosis
- https://academic.oup.com/humrep/advance-article/doi/10.1093/humrep/deaf101/8159596#google_vignette
小児期の有害体験と子宮内膜症リスク-全国コホート研究 Adverse childhood experiences and the risk of endometriosis—a nationwide cohort study
Marika Rostvall , Cecilia Magnusson , Kristina Gemzell-Danielsson , Kyriaki Kosidou , Johanna Sieurin
Human Reproduction Published:11 June 2025
DOI:https://doi.org/10.1093/humrep/deaf101
Abstract
STUDY QUESTION
Is childhood adversity associated with the subsequent diagnosis of endometriosis?
SUMMARY ANSWER
Childhood adversities, including parental substance abuse, parental intellectual disability, parental psychiatric disorder, having a teenage parent, child welfare intervention, parental separation, residential instability, receiving public assistance, exposure to violence, and parental exposure to violence were linked to a higher risk of endometriosis, and the risk increased with increasing number of adversities.
WHAT IS KNOWN ALREADY
The etiology of endometriosis is still not fully explained and there is a need for identification and greater understanding of risk factors. A few studies have previously demonstrated an association between self-reported childhood abuse and an increased risk of endometriosis.
STUDY DESIGN, SIZE, DURATION
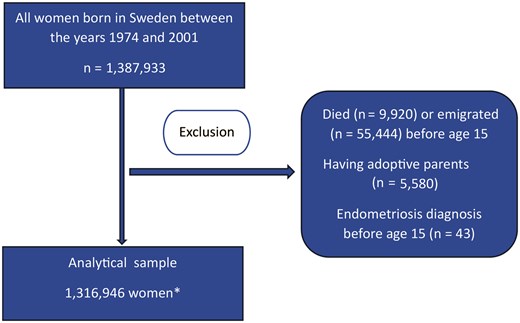
This prospective cohort study included all women born in Sweden from 1974 to 2001 using data from a linkage of several national registers. Women who died, emigrated, or received an endometriosis diagnosis before age 15 years and women who were adopted were excluded, leaving 1 316 946 women in the analytical sample. We identified 24 311 women with endometriosis based on ICD-codes registered by a health care professional. Childhood adversities were identified through a variety of different registers. Univariable and multivariable Cox proportional hazards regression models were used to estimate hazard ratios between experiencing adversities and subsequent endometriosis diagnosis.
MAIN RESULTS AND THE ROLE OF CHANCE
All the examined adversities, except familial death, were associated with an increased risk of later endometriosis diagnosis. Among the adversities associated with endometriosis risk, the strongest association observed was for exposure to violence (HR = 2.38, 95% CI 1.89–2.99) and the weakest association observed was for having a teenage parent (HR = 1.20, 95% CI 1.13–1.27). Having experienced any adversity was significantly associated with an increased risk for endometriosis diagnosis (HR = 1.20 95% CI 1.17–1.24) and the risk increased with increasing number of adversities, with an up to 60% increase in risk among those who had five or more adversities (HR = 1.61 1.37–1.88). Adjustment for covariates did not substantially influence the results.
LIMITATIONS, REASONS FOR CAUTION
Since endometriosis is widely underdiagnosed there might be many false negatives in the sample, which may introduce bias if differential.
WIDER IMPLICATIONS OF THE FINDINGS
The results of our study suggest that early life adversity is associated with an increased risk of being diagnosed with endometriosis. This finding could help guide further etiological research. It also strengthens the already large amount of evidence showing that childhood adversity has profound consequences for future health, and that there is a need for effective policies to protect children and support parents. Additionally, clinicians might need to be aware of childhood adversity as a potential risk factor for endometriosis development, and make sure to offer a thorough gynecological evaluation in individuals who have experienced childhood adversities and present with pelvic pain or dysmenorrhea.
STUDY FUNDING/COMPETING INTEREST(S)
Karolinska Institutet and Region Stockholm supported this work. The funding sources had no direct involvement. K.G.-D. reports honoraria for ad hoc participation as invited speaker or expert for Organon, Bayer, Gedeon Richter, ObsEva, Addeira, Exelgyn/Nordic, Exeltis, Cirqle, and Natural Cycles. The remaining authors report no conflict of interest.
TRIAL REGISTRATION NUMBER
N/A.