2025-08-20 ワシントン州立大学(WSU)
<関連情報>
- https://news.wsu.edu/press-release/2025/08/20/hospitals-linked-to-antibiotic-resistance-in-guatemala/
- https://www.nature.com/articles/s41598-025-03379-9
コミュニティにおける広域スペクトラムセファロスポリン耐性エンテロバクター属の定着に関連するリスク要因:コミュニティと病院における抗生物質耐性研究(ARCH)グアテマラ Risk factors associated with community colonization of extended-spectrum cephalosporin-resistant Enterobacterales from an antibiotic resistance in communities and hospitals (ARCH) study, Guatemala
Brooke M. Ramay,Mark A. Caudell,Carmen Castillo,Laura Grajeda,Lucas F. Santos,Juan Carlos Romero,Maria Renee Lopez,Sylvia Omulo,Mariangeli Freitas Ning,Guy H. Palmer,Rachel M. Smith,Carolyn T. A. Herzig,Ashley Styczynski,Celia Cordon-Rosales & Douglas R. Call
Scientific Reports Published:29 May 2025
DOI:https://doi.org/10.1038/s41598-025-03379-9
Abstract
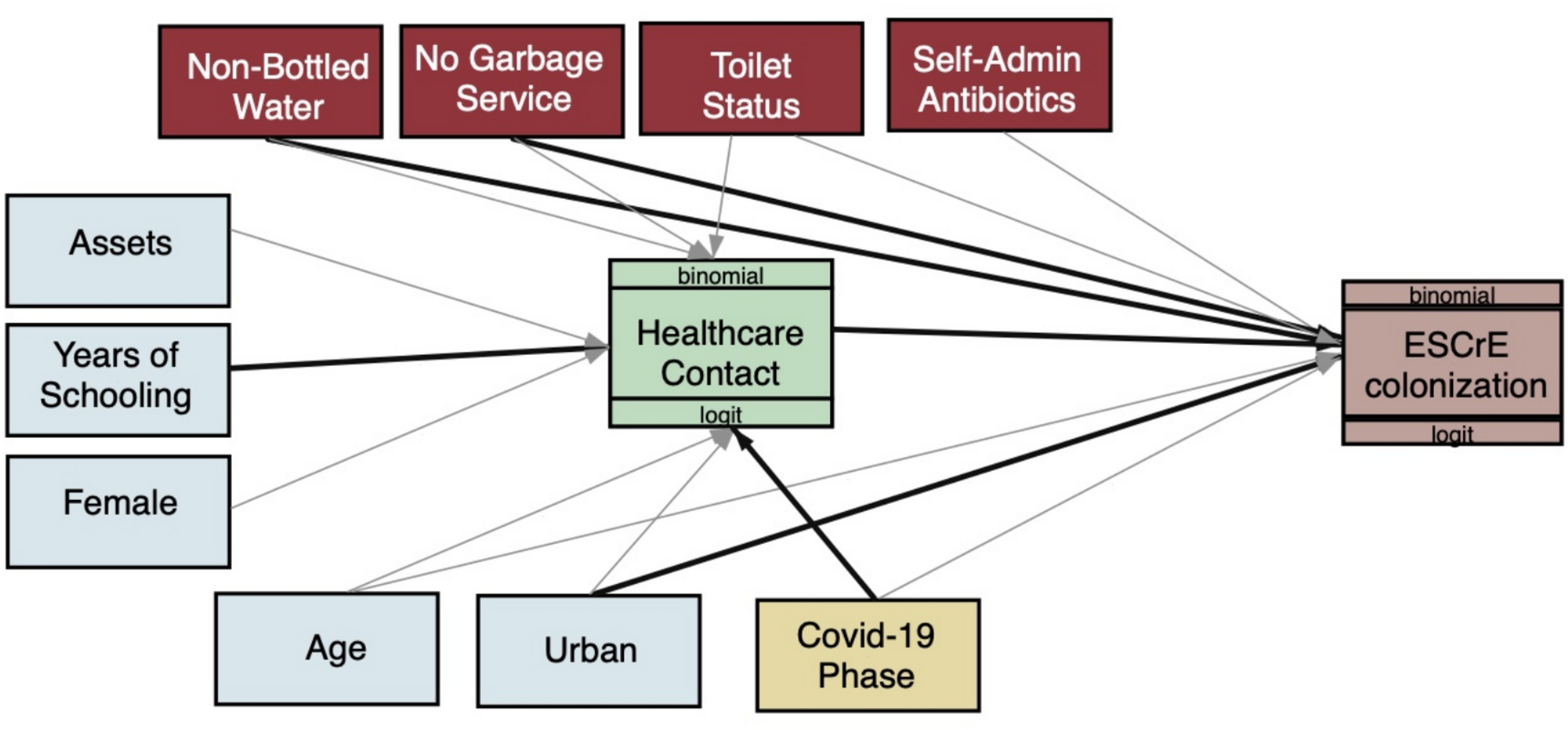
Colonization with extended-spectrum cephalosporin-resistant Enterobacterales (ESCrE) in communities may contribute to proliferation of resistance genes and drug-resistant community and hospital infections. Previous work in the Western Highlands of Guatemala found that approximately 46% of the population is colonized with these bacteria, setting the stage to identify factors that are associated with increased odds of ESCrE colonization. Stool samples and questionnaire data were collected from randomly selected participants in the catchment area of the third largest tertiary hospital in Guatemala. Logistic regression path analysis was used for this cross-sectional study to identify potential direct and indirect risk factors for colonization with ESCrE. Participants (N = 951) had a higher odds of ESCrE colonization if they had exposure to a healthcare facility within 30 days of enrollment (OR: 2.12, 95% CI = 1.19–3.77), if they resided in urban areas (OR: 1.93, 95% CI 1.09–3.42), if they did not have a service to remove household trash (OR: 1.99, 95% CI 1.11–3.58), and if the household reported drinking water from non-bottled sources (OR:1.53, 95% CI 1.0–2.33). Antibiotic self-medication was not significantly associated with the risk of colonization (OR: 1.16, 95% CI 0.65–2.06). Multiple transmission-related factors were associated with increased likelihood of ESCrE colonization, but the cross-sectional nature of this study does not distinguish factors that are correlated with an individual’s risk for colonization whence exposed. Assessing risk factors associated with colonization with antibiotic resistant bacteria may be useful for identifying mitigation strategies and evaluating the effectiveness of interventions against antibiotic resistance in community settings.