2025-10-23 慶應義塾大学医学部,理化学研究所
<関連情報>
- https://www.keio.ac.jp/ja/press-releases/2025/10/23/28-170215/
- https://www.keio.ac.jp/ja/press-releases/files/2025/10/23/251023-2.pdf
- https://www.science.org/doi/10.1126/scitranslmed.adq9913
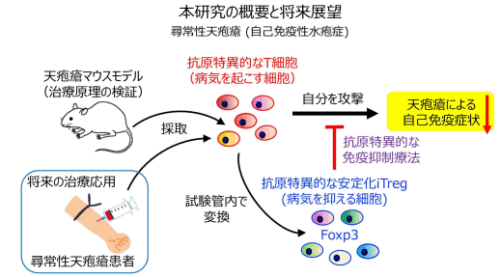
尋常性天疱瘡での抗原特異的免疫抑制を目指した病因的 T 細胞から機能的に安定な Treg 細胞への変換法 Conversion of pathogenic T cells into functionally stabilized Treg cells for antigen-specific immunosuppression in pemphigus vulgaris
Miho Mukai, Hayato Takahashi, Yoko Kubo, Yasuhiko Asahina, […] , and Masayuki Amagai
Science Translational Medicine Published:22 Oct 2025
DOI:https://doi.org/10.1126/scitranslmed.adq9913
Editor’s summary
A challenge in the development of cell therapies for many autoimmune diseases is the difficulty of achieving antigen specificity, often resulting in therapies that nonspecifically target broad swaths of the immune system and leave patients in an immunocompromised state. Autoantigen-specific regulatory T (Treg) cell therapy offers an approach to selectively quiet pathogenic immune responses, but isolating sufficient numbers of natural autoantigen-specific Treg cells from patients is challenging if not impossible. In a pair of papers, Mikami et al. and Mukai et al. adopted a new approach: turning conventional effector T cells into functional and stable Treg cells. Using a combination of cytokines and pharmacological approaches, the authors of both papers generated stable and functional induced Treg cells (S/F-iTreg cells). Mikami et al. showed that S/F-iTreg cells can be generated from several subsets of conventional T cells and are capable of suppressing inflammatory bowel disease and graft-versus-host disease in mice. Mukai et al. moved this S/F-iTreg cell generation platform one step closer to the clinic by demonstrating therapeutic efficacy in mouse models of pemphigus vulgaris and by providing proof-of-concept data that S/F-iTreg cells could be generated from cells of patients with pemphigus vulgaris. This pair of papers paves the way for a streamlined, individualized Treg cell therapy. —Courtney Malo
Abstract
Antigen-specific immunotherapy represents one candidate strategy for treating autoimmune diseases such as pemphigus vulgaris, a skin autoimmune disorder mediated by anti–desmoglein 3 (Dsg3) autoantibodies. We developed a therapeutic strategy by which Dsg3-specific pathogenic autoreactive CD4+ T cells were converted in vitro into functionally stable Foxp3+ regulatory T (Treg) cells, designated stable and functional induced Treg (S/F-iTreg) cells. The conversion was achieved by pharmacological induction of Foxp3 and costimulation-dependent installation of Treg cell–specific epigenetic changes. In an animal model of pemphigus vulgaris, the Dsg3-specific S/F-iTreg cells expanded specifically in the skin-draining lymph nodes through recognition of endogenous Dsg3. They selectively inhibited Dsg3-specific T follicular helper cell and B cell proliferation and, consequently, anti-Dsg3 autoantibody formation, without affecting the total B cell population, thereby mitigating disease progression without inducing systemic immunosuppression. Human S/F-iTreg cells with similar functions could also be efficiently generated from peripheral blood T cells of patients with pemphigus vulgaris. This study demonstrates that pathogenic autoreactive T cells can be converted into disease-specific Treg cells retaining antigen specificity, enabling antigen- and disease-specific treatment of autoimmune disease.