2025-12-01 東京科学大学
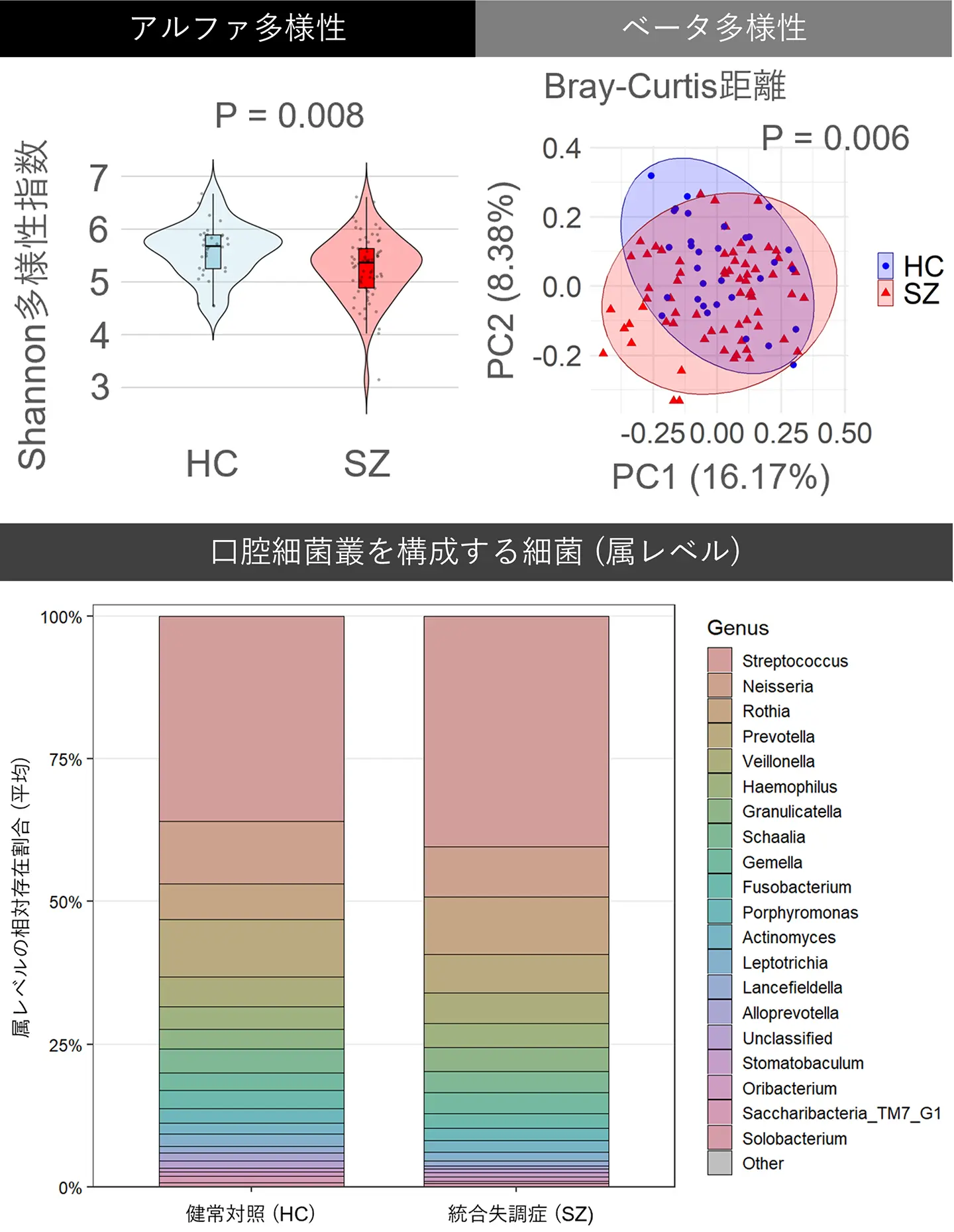
図1. 統合失調症(SZ)と健常対照(HC)の口腔細菌叢の違い。
<関連情報>
- https://www.isct.ac.jp/ja/news/alrhk8xokmzk
- https://academic.oup.com/schizophreniabulletin/advance-article-abstract/doi/10.1093/schbul/sbaf212/8346069?redirectedFrom=fulltext&login=false
統合失調症における認知障害と関連する口腔内微生物叢:構成とPICRUSt2予測機能経路 Oral Microbiota Associated With Cognitive Impairment in Schizophrenia: Composition and PICRUSt2-Predicted Functional Pathways
Takehiro Tamura, Yujin Ohsugi, Sayaka Katagiri, Ayako Kusano, Takehisa Handa, Peiya Lin, Anhao Liu, Keita Toyoshima, Shunsuke Takagi, Hiroki Shiwaku …
Schizophrenia Bulletin Published:27 November 2025
DOI:https://doi.org/10.1093/schbul/sbaf212
Abstract
Background and Hypothesis
Cognitive impairment is a core disabling feature of schizophrenia (SZ). Changes in gut microbiota have been linked to cognitive dysfunction in SZ; however, changes in the oral microbiota in relation to immune dysregulation have only been recently reported, and their relevance to cognition remains unclear. The objective of this study was to explore the relationship between oral microbiota alterations and cognitive impairment in patients with SZ and to evaluate potential mediating mechanisms, including neuroinflammation and microbial functions.
Study Design
In this cross-sectional study, we recruited 68 patients with SZ and 32 healthy controls (HC). Cognitive function was assessed using the Wechsler Adult Intelligence Scale-Fourth Edition. Oral microbiota composition was characterized by 16S rRNA gene sequencing, and microbial functions were predicted using Phylogenetic Investigation of Communities by Reconstruction of Unobserved States 2 (PICRUSt2) based on the 16S profiles. Neuroinflammation was assessed using peripheral kynurenine (KYN) pathway activity as a proxy.
Study Results
The patients with SZ exhibited significantly lower oral microbiota alpha diversity (driven by reduced evenness) and showed greater cognitive impairment and differences in the KYN pathway markers (neuroinflammation proxies) compared to HC. They also showed shifts in specific bacterial genera and the PICRUSt2-predicted functional pathways. Importantly, the oral microbiota alterations were significantly associated with cognitive impairment. Exploratory mediation analysis suggested that several pathways, including glycan biosynthesis and metabolism, may play a role in this association. In contrast, KYN pathway markers showed no significant association.
Conclusions
Our findings show an association between the oral microbiota alpha diversity and cognitive impairment in SZ, with the PICRUSt2-predicted functional pathways potentially implicated.

