2025-12-05 長寿医療研究センター研究所
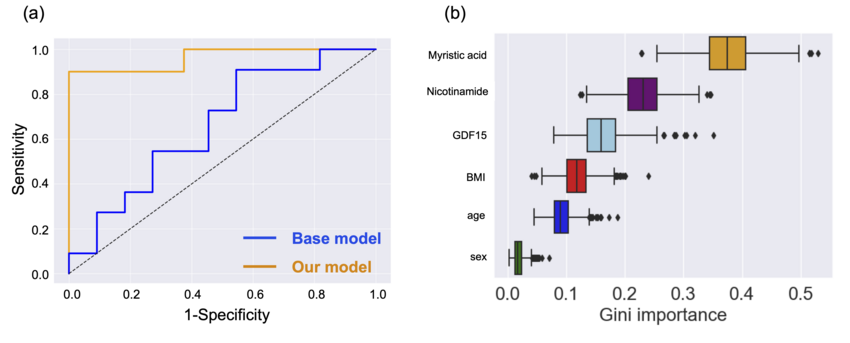
図1 予測モデルの結果
<関連情報>
- https://www.ncgg.go.jp/ri/report/20251121_press_release.html
- https://www.sciencedirect.com/science/article/pii/S1279770725002519
認知機能の虚弱性を示す血液バイオマーカーの検出に向けた統合的アプローチ An integrative approach to detecting potential blood-based biomarkers of cognitive frailty
Motoki Furutani, Mutsumi Suganuma, Tohru Hosoyama, Risa Mitsumori, Marie Takemura, Yasumoto Matsui, Yukiko Nakano, Shumpei Niida, Kouichi Ozaki, Shosuke Satake, Daichi Shigemizu
The Journal of nutrition, health and aging Available online: 24 November 2025
DOI:https://doi.org/10.1016/j.jnha.2025.100726
Highlights
- Cognitive frailty, defined by the coexistence of cognitive decline and physical frailty, presents significant health risks.
- We identified three promising biomarkers: GDF15, myristic acid, and nicotinamide.
- Low plasma myristic acid levels were crucial in predicting cognitive frailty, emphasizing their potential as a biomarker.
Abstract
Objective
Cognitive frailty, defined by the coexistence of cognitive decline and physical frailty, has been clinically defined, but its biological clues are still vague. This underscores the need for promising blood-based molecular biomarkers.
Design
Cross-sectional observational study.
Settings and participants
Frailty was diagnosed using the Japanese version of the Cardiovascular Health Study (J-CHS), and mild cognitive impairment was assessed with the Japanese version of the Montreal Cognitive Assessment (MoCA-J) and Mini-Mental State Examination-Japanese (MMSE-J). Participants with MMSE-J ≥24, MoCA-J score ≤25, and J-CHS score ≥1 were classified as having cognitive frailty. This study included 87 older adults aged ≥65 years, comprising 44 robust and 43 with cognitive frailty.
Measurements
Blood samples and associated clinical data were obtained from the National Center for Geriatrics and Gerontology Biobank in Japan. A multi-omics analysis integrating clinical data, RNA-seq, aging-related factors, and metabolomics were conducted to identify potential biomarkers through logistic regression, adjusting for age, sex, and body mass index (BMI). An optimal set of biomarkers was determined by constructing prediction models using the random forest algorithm.
Results
Three candidate biomarkers were identified from aging-related factors—growth differentiation factor (GDF15), brain-derived neurotrophic factor (BDNF), and Adiponectin—and three from metabolomics—myristic acid, nicotinamide, and γ-butyrobetaine. Using combinations of these candidates with clinical variables, we constructed risk prediction models. The best model incorporated one aging-related factors (GDF15) and two metabolites (myristic acid, and nicotinamide), achieving a high area under the receiver operating characteristic curve (AUC) of 0.96 in an independent validation cohort. This was significantly higher than models based solely on clinical information (age, sex, and BMI) (Welch’s t-test, p <0.001). Among these biomarkers, myristic acid showed the highest influence, with a median Gini importance of 0.38 (95% confidence interval: 0.29–0.47).
Conclusions
We identified three promising biomarkers—GDF15, myristic acid, and nicotinamide—for cognitive frailty. Notably, low plasma myristic acid levels emerged as the most significant contributor to the prediction model. Further refinement and large-scale validation will be essential to support its future clinical application.