2025-12-08 ミシガン大学

Geeta Peethambaran performs a static balance training exercise while wearing 13 sensors on velcro straps. Emma Nigrelli (left) spots while Wendy Carender (right) observes, wearing eye-tracking glasses. Nadine El-Ghaffir looks on. Image credit: Marcin Szczepanski, Michigan Engineering
<関連情報>
- https://news.umich.edu/ai-supports-home-based-balance-training/
- https://link.springer.com/article/10.1186/s12984-025-01760-3
- https://ieeexplore.ieee.org/document/11051035/authors
静的立位バランストレーニング運動中の強度の自動マルチIMUベースのディープラーニング評価 Automatic multi-IMU-based deep learning evaluation of intensity during static standing balance training exercises
Safa Jabri,Jeremiah Hauth,Christopher DiCesare,Wendy Carender,Lauro Ojeda,Jenna Wiens,Leia Stirling,Xun Huan & Kathleen H. Sienko
Journal of NeuroEngineering and Rehabilitation Published:27 November 2025
DOI:https://doi.org/10.1186/s12984-025-01760-3
We are providing an unedited version of this manuscript to give early access to its findings. Before final publication, the manuscript will undergo further editing. Please note there may be errors present which affect the content, and all legal disclaimers apply.
Abstract
Background
Effective balance rehabilitation requires training at an appropriate level of exercise intensity given an individual’s needs and abilities. Typically balance intensity is assessed through in-clinic visual observation by physical therapists (PTs), which limits the ability to monitor and progress intensity during home-based components of training programs. The goal of this study was to train and evaluate machine learning models for estimating physical therapists’ perceived balance exercise intensity using data from full-body wearable sensors to support the development of home-based training exercise dosage monitoring.
Methods
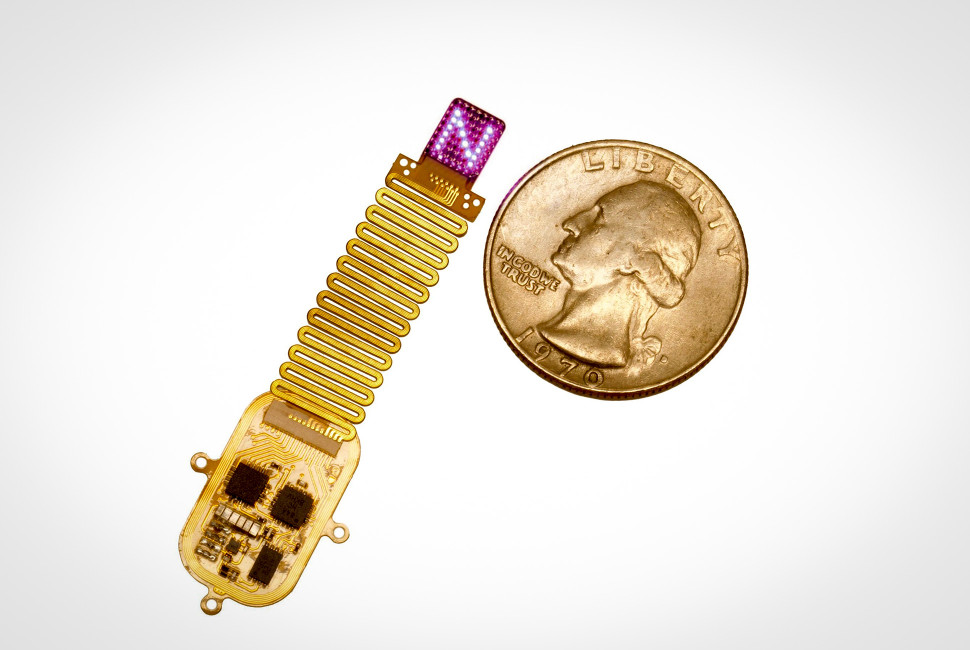
Balance exercise participants (n = 47) participated in a single-day balance training session where they were filmed performing static standing exercises at various levels of intensity. Kinematic data from 13 full-body wearable inertial measurement units (IMUs) and self-ratings of balance intensity were also collected. An additional cohort of PT participants (n = 42) was recruited to watch the videos of the balance exercise participants and provide ratings of balance intensity. The mean PT rating for each video was used as a ground truth (GT) label of balance intensity. We trained and evaluated Convolutional Neural Networks (CNN)-based models to predict balance intensity based on performance as captured through the IMUs. Model performance was evaluated by calculating the root-mean-square error (RMSE) of predications. A sensitivity analysis was also performed to assess the effect of the number of IMUs used on model performance.
Results
Models trained on orientation derived from all 13 IMUs achieved good predictive performance as indicated by a RMSE of 0.66 [0.62, 0.69], which was within the threshold defined by typical inter-rater variabilities between PTs (RMSE of 0.74 [0.72, 0.76]). Sensitivity analysis indicated that model performance stabilized at four sensors with the best performance corresponding to sensors placed on both thighs and the lower and upper back.
Conclusions
Findings from this study indicated that balance intensity assessment can be achieved through wearable sensors and a CNN model, which could support the supervision and effectiveness of home-based balance rehabilitation.
視線追跡により、立位バランスパフォーマンスを評価する際の理学療法士の意思決定が明らかになる Eye Tracking Reveals Physical Therapist Decision Making While Evaluating Standing Balance Performance
Emma Nigrelli; Wendy Carender; Kathleen H. Sienko; Leia Stirling
IEEE Transactions on Neural Systems and Rehabilitation Engineering Published:25 June 2025
DOI:https://doi.org/10.1109/TNSRE.2025.3582571
Abstract
Physical therapists (PTs) play an important role in balance rehabilitation as they make observations of patients to aid their decision making. Eye tracking can provide a record of these observations. Prior work has used eye tracking to compare PTs’ visual behaviors across different experience levels; however, these studies have not considered how PTs’ visual behaviors change with respect to patients’ performances. This study aimed to identify the regions of the body PT participants focused on while evaluating standing balance and whether these regions of interest change with different observed levels of balance performance. Eleven pairs of older adults and PTs participated. The PT participants wore eye tracking glasses while watching the older adult participants perform standing balance exercises and provided performance ratings. Areas of interest, including the head, torso, upper extremities (UE), and lower extremities (LE), were defined to quantify the number and average duration of visits. PTs had the most and longest visits to the LE and the fewest and shortest visits to the UE across all ratings. As balance performance worsened, PTs increased the number of visits to the head, while decreasing the average visit duration to the torso and LE. These results suggest lower body balance strategies are important visual characteristics PTs consider while evaluating balance performance and, as exercises become more challenging, PTs demonstrate increasingly rapid visual scans of the whole-body to continually update their understanding of performance. This understanding of PT visual behaviors has implications for the future development of PT-informed balance assessment models.