- 真菌感染症は毎年150万人以上の死者を出し、それを予防するワクチンはない
Fungal infections cause 1.5M+ deaths each year, and there’s no vaccine to prevent them
- アスペルギルス症、カンジダ症およびニューモシスト症の前臨床モデルにおける汎真菌ワクチンの免疫原性と保護効果 Immunogenicity and protective efficacy of a pan-fungal vaccine in preclinical models of aspergillosis, candidiasis, and pneumocystosis
- 米国におけるリスク条件と侵襲性真菌症における死亡率の推移(1999年~2018年 Mortality Trends in Risk Conditions and Invasive Mycotic Disease in the United States, 1999-2018
- 米国における真菌感染症の有病率と医療負担の推移(2018年版)Prevalence and Healthcare Burden of Fungal Infections in the United States, 2018
真菌感染症は毎年150万人以上の死者を出し、それを予防するワクチンはない Fungal infections cause 1.5M+ deaths each year, and there’s no vaccine to prevent them
2023-01-31 ジョージア大学 (UGA)
◆真菌感染症は、世界中で毎年150万人以上の死者を出し、何十億もの費用がかかっています。また、UGAの過去の研究によると、真菌感染症は入院費用を2倍にし、入院期間を2倍にし、入院患者の死亡リスクを2倍にする。しかし、現在のところ、真菌感染症から弱い立場の患者を守るための有効なワクチンは存在しない。
◆この実験用ワクチンは、致死的真菌感染症の80%以上の原因である、最も一般的な3つの真菌病原体から守るように設計されています。この研究では、非ヒト霊長類を含む4つの前臨床動物モデルでワクチンの有効性を検証しました。
◆研究者らは、移植患者やHIV患者、がん患者など、最も感染リスクの高い人々の薬物療法に類似した、さまざまな免疫抑制モデルを用いて研究を行った。このワクチンは、それぞれのモデルにおいて、防御抗体の形成に有効であった。
◆真菌感染症は、コントロールされていないHIVや、化学療法や抗炎症剤などの治療で免疫力が低下した人など、免疫障害を持つ人に最もよく見られるものです。
◆しかし、ノリス、博士研究員エミリー・レイエンスと2022年の公衆衛生大学のホセ・コルデロからの以前の研究は、そのリスクのある人口が近年拡大していることを示しました。その研究は、糖尿病、慢性閉塞性肺疾患(またはCOPD)、またはCOVID-19、結核やインフルエンザなどの共同感染症を持つ人々は同様に真菌感染症を発症するリスクが高いことを示しています。
◆この新しいワクチンは、真菌感染症の最も一般的な3つの原因を対象としています。アスペルギルス、カンジダ、ニューモシスチスです。特にカンジダは、さまざまな菌種が多剤耐性を持つようになったため、医療界で懸念が高まっています。
◆このワクチンは、動物モデルで幅広い抗真菌性免疫を示し、将来の臨床試験に向けて良い兆しを見せています。
<関連情報>
- https://news.uga.edu/new-vaccine-targets-fungal-infections/
- https://academic.oup.com/pnasnexus/article/1/5/pgac248/6798391?login=false
- https://pubmed.ncbi.nlm.nih.gov/33876235/
- https://pubmed.ncbi.nlm.nih.gov/35036461/
アスペルギルス症、カンジダ症およびニューモシスト症の前臨床モデルにおける汎真菌ワクチンの免疫原性と保護効果 Immunogenicity and protective efficacy of a pan-fungal vaccine in preclinical models of aspergillosis, candidiasis, and pneumocystosis
Emily Rayens, Whitney Rabacal, Hubertine M E Willems, Gabrielle M Kirton, James P Barber, Jarrod J Mousa, Brandi N Celia-Sanchez, Michelle Momany, Karen A Norris
PNAS Nexus Published:04 November 2022
DOI:https://doi.org/10.1093/pnasnexus/pgac248
Abstract
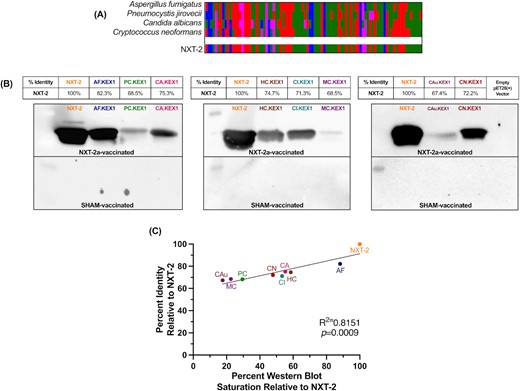
Invasive fungal infections cause over 1.5 million deaths worldwide. Despite increases in fungal infections as well as the numbers of individuals at risk, there are no clinically approved fungal vaccines. We produced a “pan-fungal” peptide, NXT-2, based on a previously identified vaccine candidate and homologous sequences from Pneumocystis, Aspergillus,Candida, and Cryptococcus. We evaluated the immunogenicity and protective capacity of NXT-2 in murine and nonhuman primate models of invasive aspergillosis, systemic candidiasis, and pneumocystosis. NXT-2 was highly immunogenic and immunized animals had decreased mortality and morbidity compared to nonvaccinated animals following induction of immunosuppression and challenge with Aspergillus, Candida, or Pneumocystis. Data in multiple animal models support the concept that immunization with a pan-fungal vaccine prior to immunosuppression induces broad, cross-protective antifungal immunity in at-risk individuals.
米国におけるリスク条件と侵襲性真菌症における死亡率の推移(1999年~2018年 Mortality Trends in Risk Conditions and Invasive Mycotic Disease in the United States, 1999-2018
Emily Rayens , Karen A Norris , José F Cordero
National Library of Medicin Published:2022 Jan 29
DOI:https://doi.org/10.1093/cid/ciab336
Abstract
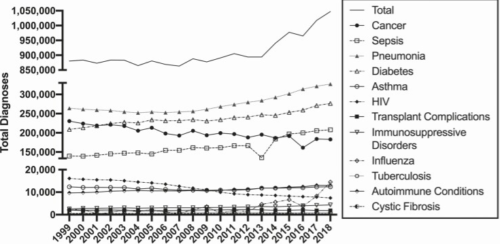
Background: Invasive fungal infections in the United States are chronically underdiagnosed and a lack of coordinated surveillance makes the true burden of disease difficult to determine. The purpose of this analysis was to capture mortality-associated burden of risk conditions and fungal infections.
Methods: We analyzed data from the National Vital Statistics System from 1999 through 2018 to estimate the mortality attributed to risk conditions and related fungal disease.
Results: The number of risk conditions associated with fungal disease is steadily rising in the United States, with 1 047 422 diagnoses at time of death in 2018. While fungal disease decreased substantially from 1999 to 2010, primarily due to the control of human immunodeficiency virus (HIV) infection, the number of deaths with fungal diagnosis has increased in the non-HIV cohort, with significant increases in patients with diabetes, cancer, immunosuppressive disorders, or sepsis.
Conclusions: The landscape of individuals at risk for serious fungal diseases is changing, with a continued decline in HIV-associated incidence but increased diagnoses in patients with cancer, sepsis, immunosuppressive disorders, and influenza. Additionally, there is an overall increase in the number of fungal infections in recent years, indicating a failure to control fungal disease mortality in these new immunocompromised cohorts. Improvement in the prevention and management of fungal diseases is needed to control morbidity and mortality in the rising number of immunocompromised and at-risk patients in the United States.
米国における真菌感染症の有病率と医療負担の推移(2018年版)Prevalence and Healthcare Burden of Fungal Infections in the United States, 2018
Emily Rayens , Karen A Norris
National Library of Medicin Published:2022 Jan 10
DOI:https://doi.org/10.1093/ofid/ofab593
Abstract
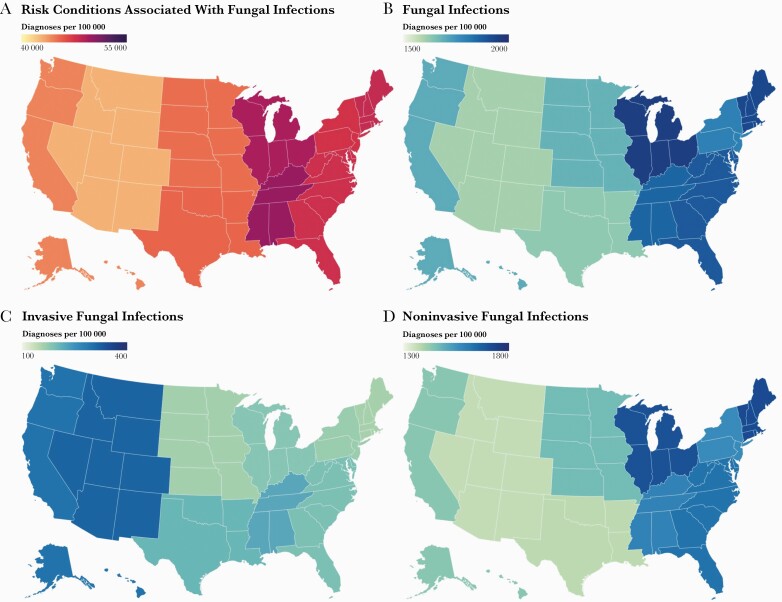
Background: Fungal infections are responsible for >1.5 million deaths globally per year, primarily in those with compromised immune function. This is concerning as the number of immunocompromised patients, especially in those without human immunodeficiency virus (HIV), has risen in the past decade. The purpose of this analysis was to provide the current prevalence and impact of fungal disease in the United States.
Methods: We analyzed hospital discharge data from the most recent (2018) Healthcare Cost and Utilization Project National Inpatient Sample, and outpatient visit data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey. Costs are presented in 2018 United States (US) dollars.
Results: In the 35.5 million inpatient visits documented in 2018 in the US, approximately 666 235 fungal infections were diagnosed, with an estimated attributable cost of $6.7 billion. Aspergillus, Pneumocystis, and Candida infections accounted for 76.3% of fungal infections diagnosed, and 81.1% of associated costs. Most fungal disease occurred in patients with elevated risk of infection. The visit costs, lengths of stay, and risks of mortality in this population were more than twice that of those without fungal diagnoses. A further 6.6 million fungal infections were diagnosed during outpatient visits.
Conclusions: Fungal disease is a serious clinical concern with substantial healthcare costs and significant increases in morbidity and mortality, particularly among predisposed patients. Increased surveillance, standardized treatment guidelines, and improvement in diagnostics and therapeutics are needed to support the rising numbers of at-risk patients.


