2025-06-13 東京大学
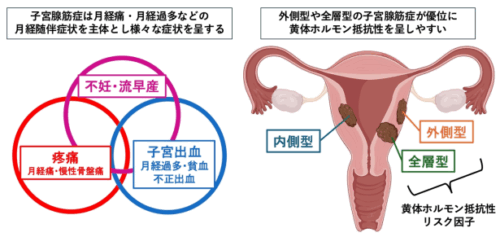
子宮腺筋症の症状と黄体ホルモン抵抗性リスク因子
<関連情報>
- https://www.h.u-tokyo.ac.jp/press/20250613.html
- https://www.h.u-tokyo.ac.jp/press/__icsFiles/afieldfile/2025/06/13/release_20250613.pdf
- https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-025-03817-w
症候性子宮腺筋症におけるプロゲステロン抵抗性の予後因子:病変局在がレボノルゲストレル子宮内システムの治療成績に及ぼす影響 Prognostic factors of progesterone resistance in symptomatic adenomyosis: impact of lesion localization on treatment outcome of levonorgestrel intrauterine system
Daiki Hiratsuka,Mitsunori Matsuo,Chihiro Ishizawa,Yamato Fukui,Takehiro Hiraoka,Shizu Aikawa,Gentaro Izumi,Miyuki Harada,Osamu Wada-Hiraike,Yutaka Osuga & Yasushi Hirota
BMC Women’s Health Published:13 June 2025
DOI:https://doi.org/10.1186/s12905-025-03817-w
Abstract
Adenomyosis often causes dysmenorrhea in women of reproductive age. Progestins such as levonorgestrel intrauterine system (LNG-IUS) are often used for treatment, but some patients experience progesterone resistance, showing poor treatment response. However, the clinical characteristics of progesterone-resistant and progesterone-sensitive patients with symptomatic adenomyosis remain unclear. We analyzed data of 69 patients with adenomyosis treated with LNG-IUS. Dysmenorrhea was quantified using linear visual analog scale (VAS) scoring, and progesterone resistance was interpreted as continued dysmenorrhea during LNG-IUS treatment. The rate of change in VAS scores of dysmenorrhea was calculated: patients with the bottom 25% improvement were defined as progesterone-resistant group, and those with the top 25% improvement as progesterone-sensitive group. The localization of adenomyosis lesions was evaluated by magnetic resonance imaging (MRI) and classified as advanced (localized in all layers of the myometrium), extrinsic (localized on the uterine serosa side), and intrinsic (localized on the endometrial side) subtypes. Progesterone-resistant group had a significantly lower incidence of intrinsic adenomyosis (7.7% vs. 69.2%, p = 0.004) and a tendency toward a higher incidence of advanced adenomyosis (61.5% vs. 23.1%, p = 0.111) compared with progesterone-sensitive group. Progesterone-sensitive group showed significant improvement of dysmenorrhea 1 month after starting LNG-IUS treatment (p < 0.001). These findings indicate that the responsiveness to LNG-IUS treatment can be determined 1 month after starting the treatment and that intrinsic adenomyosis is a favorable prognostic factor for progestin treatment with LNG-IUS, while advanced and extrinsic adenomyosis are predictors for progesterone resistance.


