2025-12-02 マウントサイナイ医療システム(MSHS)
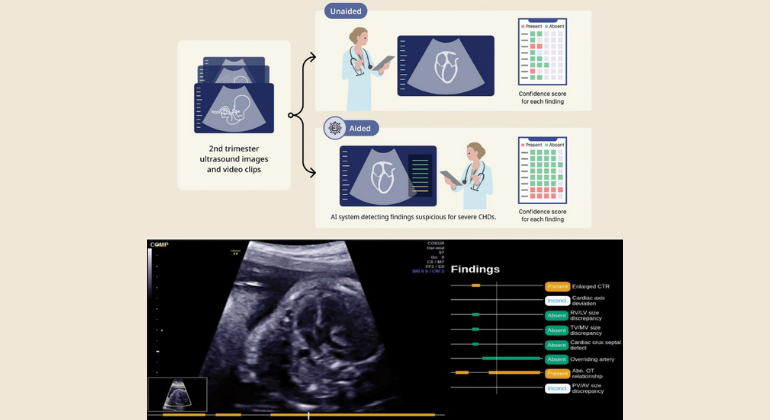
Photo credit: Figure 1AB. Courtesy of The Green Journal/Obstetrics & Gynecology
<関連情報>
- https://www.mountsinai.org/about/newsroom/2025/mount-sinai-obstetricians-first-in-new-york-city-to-use-fda-approved-ai-tool-that-enhances-fetal-screenings-for-congenital-heart-defects
- https://journals.lww.com/greenjournal/fulltext/9900/use_of_artificial_intelligence_based_software_to.1387
胎児の先天性心疾患に関連する超音波所見の特定を支援する人工知能ベースのソフトウェアの使用 Use of Artificial Intelligence–Based Software to Aid in the Identification of Ultrasound Findings Associated With Fetal Congenital Heart Defects
Lam-Rachlin、Jennifer MD; Punn、Rajesh MD; Behera、Sarina K. MD; Geiger、Miwa MD; Lachaud、Matthias MD; David、Nadine MD; Garmel、Sara MD; Fox、Nathan S. MD; Rebarber、Andrei MD; DeVore、Greggory R. MD; Zelop、Carolyn M. MD; Janssen、Matthew K. MD; Sylvester-Armstrong、Kendra R. MD; Kennedy、John MD; Spiegelman、Jessica MD; Heiligenstein、Mia MD; Bessis、Roger MD; Mobeen、Sadia MD; Kia、Farnaaz MD; Friedman、Caroline MD; Melka、Stephanie; Stos、Bertrand MD; De Boisredon、Malo MSc; Askinazi、Eric MSc; Thorey, Valentin MSc; Gardella, Christophe PhD; Levy, Marilyne MD; Arunamata, Alisa MD
Obstetrics & Gynecology Published:October 16, 2025
DOI:10.1097/AOG.0000000000006087
Abstract
OBJECTIVE:
To evaluate whether artificial intelligence (AI)–based software was associated with enhanced identification of eight second-trimester fetal ultrasound findings suspicious for congenital heart defects (CHDs) among obstetrician–gynecologists (ob-gyns) and maternal–fetal medicine specialists.
METHODS:
A dataset of 200 fetal ultrasound examinations from 11 centers, including 100 with at least one suspicious finding, was retrospectively constituted (singleton pregnancy, 18–24 weeks of gestation, patients aged 18 years or older). Only examinations containing two-dimensional grayscale cines with interpretable four-chamber, left ventricular outflow tract, and right ventricular outflow tract standard views were included. Seven ob-gyns and seven maternal–fetal medicine specialists reviewed each examination in randomized order both with and without AI assistance and assessed the presence or absence of each finding suspicious for CHD with confidence scores. Outcomes included readers’ performance in identifying the presence of any finding and each finding at the examination level, as measured by the area under the receiver operating characteristic curve (AUROC), sensitivity, and specificity. In addition, reading time and confidence were evaluated.
RESULTS:
The detection of any suspicious finding significantly improved for AI-aided compared with unaided readers with a significantly higher AUROC (0.974 [95% CI, 0.957–0.990] vs 0.825 [95% CI, 0.741–0.908], P=.002), sensitivity (0.935 [95% CI, 0.892–0.978] vs 0.782 [95% CI, 0.686–0.878]), and specificity (0.970 [95% CI, 0.949–0.991] vs 0.759 [95% CI, 0.630–0.887]). AI assistance also resulted in a significant decrease in clinician interpretation time and increase in clinician confidence score (226 seconds [95% CI, 218–234] vs 274 seconds [95% CI, 265–283], P<.001; 4.63 [95% CI, 4.60–4.66] vs 3.90 [95% CI, 3.85–3.95], P<.001, respectively).
CONCLUSION:
The use of AI-based software to assist clinicians was associated with enhanced identification of findings suspicious for CHD on prenatal ultrasonography.