2026-02-04 ワシントン大学セントルイス校
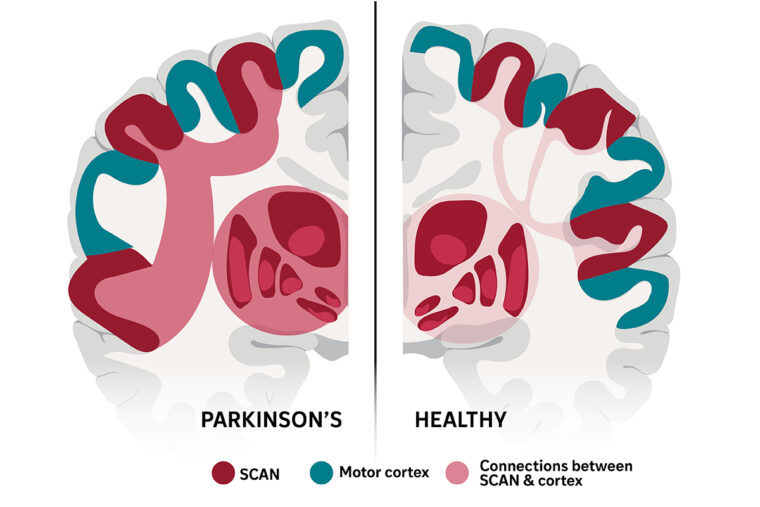
The brain network that links thinking with movement, called SCAN, was first described by WashU Medicine researchers in 2023 and has been identified in a new study as the neurological basis of Parkinson’s disease. An experimental therapy that targeted this network more than doubled symptom improvement in a small group of patients with Parkinson’s, which is characterized by hyperconnectivity (left side of illustration) between SCAN and the brain’s subcortex. (Image: Sara Moser/WashU Medicine)
<関連情報>
- https://source.washu.edu/2026/02/brain-network-responsible-for-parkinsons-disease-identified/
- https://medicine.washu.edu/news/brain-network-responsible-for-parkinsons-disease-identified/
- https://www.nature.com/articles/s41586-025-10059-1
パーキンソン病は体性認知行動ネットワーク障害である Parkinson’s disease as a somato-cognitive action network disorder
Jianxun Ren,Wei Zhang,Louisa Dahmani,Evan M. Gordon,Shenshen Li,Ying Zhou,Yang Long,Jianting Huang,Yafei Zhu,Ning Guo,Changqing Jiang,Feng Zhang,Yan Bai,Wei Wei,Yaping Wu,Alan Bush,Matteo Vissani,Luhua Wei,Carina R. Oehrn,Melanie A. Morrison,Ying Zhu,Chencheng Zhang,Qingyu Hu,Yilin Yin,… Hesheng Liu
Nature Published:04 February 2026
DOI:https://doi.org/10.1038/s41586-025-10059-1
Abstract
Parkinson’s disease (PD) is an incurable neurological disorder that often begins insidiously with sleep disturbances and somatic symptoms, progressing to whole-body motor and cognitive symptoms1,2,3,4,5. Dysfunction of the somato-cognitive action network (SCAN)—which is thought to control action execution6,7 by coordinating arousal, organ physiology and whole-body motor plans with behavioural motivation—is a potential contributor to the diverse clinical manifestations of PD. To investigate the role of the SCAN in PD pathophysiology and treatments (medications, deep-brain stimulation (DBS), transcranial magnetic stimulation (TMS) and MRI-guided focused ultrasound stimulation (MRgFUS)), we built a large (n = 863), multimodal, multi-intervention clinical imaging dataset. Resting-state functional connectivity revealed that the substantia nigra and all PD DBS targets (subthalamic nucleus, globus pallidus and ventral intermediate thalamus) are selectively connected to the SCAN rather than to effector-specific motor regions. Importantly, PD was characterized by specific hyperconnectivity between the SCAN and the subcortex. We therefore followed six PD cohorts undergoing DBS, TMS, MRgFUS and levodopa therapy using precision resting-state functional connectivity and electrocorticography recording. Efficacious treatments reduced SCAN-to-subcortex hyperconnectivity. Targeting the SCAN instead of effector regions doubled the efficacy of TMS treatments. Focused ultrasound treatment benefits increased when the target was closer to the thalamic SCAN sweet spot. Thus, SCAN hyperconnectivity is central to PD pathophysiology and its alleviation is a hallmark of successful neuromodulation. Targeting functionally defined subcortical SCAN nodes may improve existing therapies (DBS, MRgFUS), whereas cortical SCAN targets offer effective non-invasive or minimally invasive neuromodulation for PD.

