2022-09-08 スウェーデン・リンショーピング大学
今回の研究では、リンショーピン大学の研究者らが、重度のCOVID-19感染が身体の免疫細胞に長期的な影響を与えるかどうかを調べた。
研究チームは、ノルショーピングのVrinnevi病院で治療を受けたCOVID-19患者46人と、健康な対照被験者31人を対象に調査を行った。研究者らは、入院時に患者から採取した血液サンプルと、2週間後、6週間後、6〜8ヵ月後に採取した血液サンプルを分析した。彼らは、ウイルス特異的T細胞の特性を調べるだけでなく、この病気がすべてのT細胞に一般的な影響を及ぼしているかどうかも調べた。
この研究では、すべての患者がSARS-CoV-2に対する抗体を獲得したことが確認された。これらの抗体のレベルは、6カ月後に低下し始めました
<関連情報>
- https://liu.se/en/news-item/svar-covid-19-ger-langvariga-negativa-effekter-pa-immunforsvaret
- https://www.frontiersin.org/articles/10.3389/fimmu.2022.931039/full
COVID-19の入院後、少なくとも6ヶ月間はT細胞の異常が持続する。
T cell perturbations persist for at least 6 months following hospitalization for COVID-19
Melissa Govender, Francis R. Hopkins, Robin Göransson, Cecilia Svanberg, Esaki M. Shankar, Maria Hjorth, Åsa Nilsdotter-Augustinsson, Johanna Sjöwall, Sofia Nyström and Marie Larsson
Frontiers in Immunology Published:08 August 2022
DOI:https://doi.org/10.3389/fimmu.2022.931039
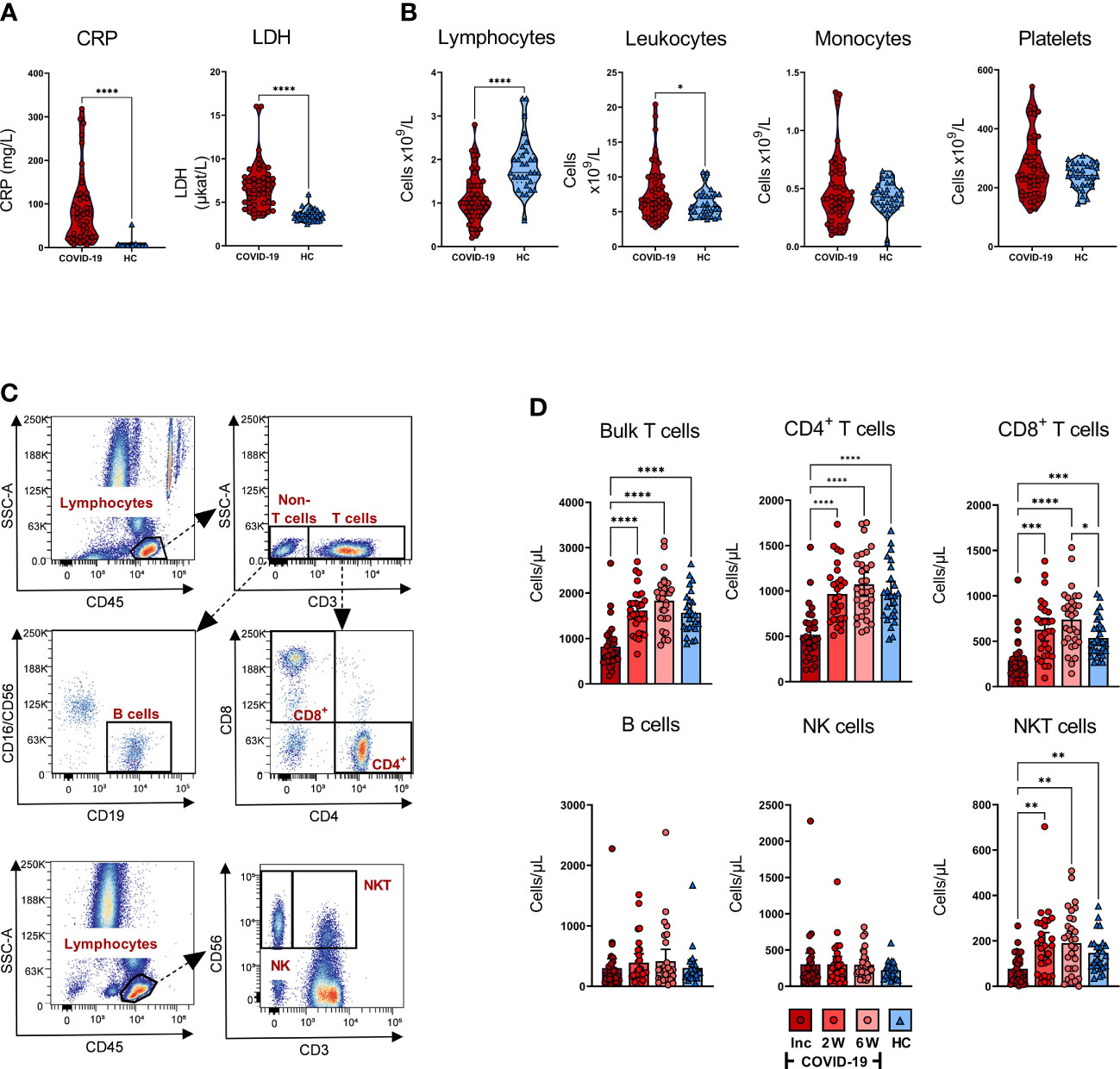
COVID-19 is being extensively studied, and much remains unknown regarding the long-term consequences of the disease on immune cells. The different arms of the immune system are interlinked, with humoral responses and the production of high-affinity antibodies being largely dependent on T cell immunity. Here, we longitudinally explored the effect COVID-19 has on T cell populations and the virus-specific T cells, as well as neutralizing antibody responses, for 6-7 months following hospitalization. The CD8+ TEMRA and exhausted CD57+ CD8+ T cells were markedly affected with elevated levels that lasted long into convalescence. Further, markers associated with T cell activation were upregulated at inclusion, and in the case of CD69+ CD4+ T cells this lasted all through the study duration. The levels of T cells expressing negative immune checkpoint molecules were increased in COVID-19 patients and sustained for a prolonged duration following recovery. Within 2-3 weeks after symptom onset, all COVID-19 patients developed anti-nucleocapsid IgG and spike-neutralizing IgG as well as SARS-CoV-2-specific T cell responses. In addition, we found alterations in follicular T helper (TFH) cell populations, such as enhanced TFH-TH2 following recovery from COVID-19. Our study revealed significant and long-term alterations in T cell populations and key events associated with COVID-19 pathogenesis.