初産が早いこと、生殖回数が多いこと、生理開始年齢が若いことは、心血管障害のリスク上昇につながる可能性がある。 An earlier first birth, a higher number of live births, and starting periods at a younger age may be linked to higher risk of cardiovascular problems.
2023-02-27 インペリアル・カレッジ・ロンドン(ICL)
<関連情報>
- https://www.imperial.ac.uk/news/243393/reproductive-factors-women-contribute-risk-cardiovascular/
- https://www.ahajournals.org/doi/10.1161/JAHA.122.027933
性特異的生殖因子は女性の心血管疾患リスクを増大させる:メンデルランダム化研究 Sex‐Specific Reproductive Factors Augment Cardiovascular Disease Risk in Women: A Mendelian Randomization Study
Maddalena Ardissino,Eric A. W. Slob,Paul Carter,Tormod Rogne,Joanna Girling,Stephen Burgess and Fu Siong Ng
Journal of the American Heart Association Published:27 Feb 2023
DOI:https://doi.org/10.1161/JAHA.122.027933
Abstract
Background
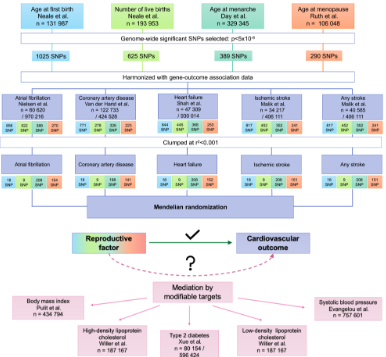
Observational studies suggest that reproductive factors are associated with cardiovascular disease, but these are liable to influence by residual confounding. This study explores the causal relevance of reproductive factors on cardiovascular disease in women using Mendelian randomization.
Methods and Results
Uncorrelated (r2<0.001), genome‐wide significant (P<5×10-8) single‐nucleotide polymorphisms were extracted from sex‐specific genome‐wide association studies of age at first birth, number of live births, age at menarche, and age at menopause. Inverse‐variance weighted Mendelian randomization was used for primary analyses on outcomes of atrial fibrillation, coronary artery disease, heart failure, ischemic stroke, and stroke. Earlier genetically predicted age at first birth increased risk of coronary artery disease (odds ratio [OR] per year, 1.49 [95% CI, 1.28–1.74], P=3.72×10-7) heart failure (OR, 1.27 [95% CI, 1.06–1.53], P=0.009), and stroke (OR, 1.25 [95% CI, 1.00–1.56], P=0.048), with partial mediation through body mass index, type 2 diabetes, blood pressure, and cholesterol traits. Higher genetically predicted number of live births increased risk of atrial fibrillation (OR for <2, versus 2, versus >2 live births, 2.91 [95% CI, 1.16–7.29], P=0.023), heart failure (OR, 1.90 [95% CI, 1.28–2.82], P=0.001), ischemic stroke (OR, 1.86 [95% CI, 1.03–3.37], P=0.039), and stroke (OR, 2.07 [95% CI, 1.22–3.52], P=0.007). Earlier genetically predicted age at menarche increased risk of coronary artery disease (OR per year, 1.10 [95% CI, 1.06–1.14], P=1.68×10-6) and heart failure (OR, 1.12 [95% CI, 1.07–1.17], P=5.06×10-7); both associations were at least partly mediated by body mass index.
Conclusions
These results support a causal role of a number of reproductive factors on cardiovascular disease in women and identify multiple modifiable mediators amenable to clinical intervention.