2024-02-20 ラトガース大学
<関連情報>
- https://www.rutgers.edu/news/drug-repairs-systems-remove-alzheimers-causing-waste-brain-study-shows
- https://www.jci.org/articles/view/171468
- https://www.nature.com/articles/s41586-021-03489-0
- https://www.nature.com/articles/nature14432
Piezo1アゴニストが頭蓋砕骨症および老化マウスにおいて髄膜リンパ管、ドレナージ、脳-CSF灌流を回復させる Piezo1 agonist restores meningeal lymphatic vessels, drainage, and brain-CSF perfusion in craniosynostosis and aged mice
Matt J. Matrongolo, Phillip S. Ang, Junbing Wu, Aditya Jain, Joshua K. Thackray, Akash Reddy, Chi Chang Sung, Gaëtan Barbet, Young-Kwon Hong, and Max A. Tischfield
Journal of Clinical Investigation Published November 2, 2023
DOI:https://doi.org/10.1172/JCI171468
Abstract
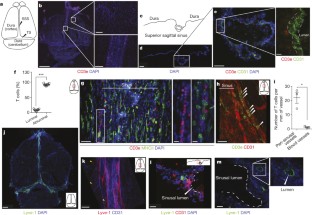
Skull development coincides with the onset of cerebrospinal fluid (CSF) circulation, brain-CSF perfusion, and meningeal lymphangiogenesis, processes essential for brain waste clearance. How these processes are affected by craniofacial disorders such as craniosynostosis are poorly understood. We report that raised intracranial pressure and diminished CSF flow in craniosynostosis mouse models associate with pathological changes to meningeal lymphatic vessels that affect their sprouting, expansion, and long-term maintenance. We also show that craniosynostosis affects CSF circulatory pathways and perfusion into the brain. Further, craniosynostosis exacerbates amyloid pathology and plaque buildup in Twist1+/–:5xFAD transgenic Alzheimer’s disease models. Treating craniosynostosis mice with Yoda1, a small molecule agonist for Piezo1, reduces intracranial pressure and improves CSF flow, in addition to restoring meningeal lymphangiogenesis, drainage to the deep cervical lymph nodes, and brain-CSF perfusion. Leveraging these findings, we show that Yoda1 treatments in aged mice with reduced CSF flow and turnover improve lymphatic networks, drainage, and brain-CSF perfusion. Our results suggest that CSF provides mechanical force to facilitate meningeal lymphatic growth and maintenance. Additionally, applying Yoda1 agonist in conditions with raised intracranial pressure and/or diminished CSF flow, as seen in craniosynostosis or with ageing, is a possible therapeutic option to help restore meningeal lymphatic networks and brain-CSF perfusion.
Graphical Abstract

髄膜リンパ管はミクログリア応答と抗Aβ免疫療法に影響する Meningeal lymphatics affect microglia responses and anti-Aβ immunotherapy
Sandro Da Mesquita,Zachary Papadopoulos,Taitea Dykstra,Logan Brase,Fabiana Geraldo Farias,Morgan Wall,Hong Jiang,Chinnappa Dilip Kodira,Kalil Alves de Lima,Jasmin Herz,Antoine Louveau,Dylan H. Goldman,Andrea Francesca Salvador,Suna Onengut-Gumuscu,Emily Farber,Nisha Dabhi,Tatiana Kennedy,Mary Grace Milam,Wendy Baker,Igor Smirnov,Stephen S. Rich,Dominantly Inherited Alzheimer Network,Bruno A. Benitez,Celeste M. Karch,… Jonathan Kipnis
Nature Published28 April 2021
DOI:https://doi.org/10.1038/s41586-021-03489-0

Abstract
Alzheimer’s disease (AD) is the most prevalent cause of dementia1. Although there is no effective treatment for AD, passive immunotherapy with monoclonal antibodies against amyloid beta (Aβ) is a promising therapeutic strategy2,3. Meningeal lymphatic drainage has an important role in the accumulation of Aβ in the brain4, but it is not known whether modulation of meningeal lymphatic function can influence the outcome of immunotherapy in AD. Here we show that ablation of meningeal lymphatic vessels in 5xFAD mice (a mouse model of amyloid deposition that expresses five mutations found in familial AD) worsened the outcome of mice treated with anti-Aβ passive immunotherapy by exacerbating the deposition of Aβ, microgliosis, neurovascular dysfunction, and behavioural deficits. By contrast, therapeutic delivery of vascular endothelial growth factor C improved clearance of Aβ by monoclonal antibodies. Notably, there was a substantial overlap between the gene signature of microglia from 5xFAD mice with impaired meningeal lymphatic function and the transcriptional profile of activated microglia from the brains of individuals with AD. Overall, our data demonstrate that impaired meningeal lymphatic drainage exacerbates the microglial inflammatory response in AD and that enhancement of meningeal lymphatic function combined with immunotherapies could lead to better clinical outcomes.
中枢神経系リンパ管の構造と機能的特徴 Structural and functional features of central nervous system lymphatic vessels
Antoine Louveau,Igor Smirnov,Timothy J. Keyes,Jacob D. Eccles,Sherin J. Rouhani,J. David Peske,Noel C. Derecki,David Castle,James W. Mandell,Kevin S. Lee,Tajie H. Harris &Jonathan Kipnis
Nature Published:01 June 2015
DOI:https://doi.org/10.1038/nature14432
Abstract
One of the characteristics of the central nervous system is the lack of a classical lymphatic drainage system. Although it is now accepted that the central nervous system undergoes constant immune surveillance that takes place within the meningeal compartment1,2,3, the mechanisms governing the entrance and exit of immune cells from the central nervous system remain poorly understood4,5,6. In searching for T-cell gateways into and out of the meninges, we discovered functional lymphatic vessels lining the dural sinuses. These structures express all of the molecular hallmarks of lymphatic endothelial cells, are able to carry both fluid and immune cells from the cerebrospinal fluid, and are connected to the deep cervical lymph nodes. The unique location of these vessels may have impeded their discovery to date, thereby contributing to the long-held concept of the absence of lymphatic vasculature in the central nervous system. The discovery of the central nervous system lymphatic system may call for a reassessment of basic assumptions in neuroimmunology and sheds new light on the aetiology of neuroinflammatory and neurodegenerative diseases associated with immune system dysfunction.