2024-08-06 カリフォルニア大学サンディエゴ校(UCSD)
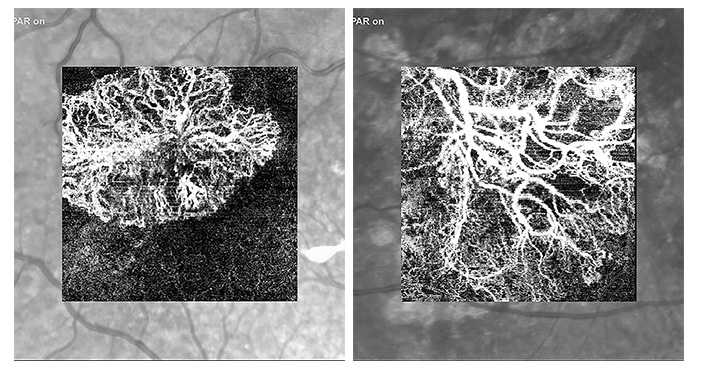
OCTA images from eye vasculature impacted by age-related macular degeneration (AMD) at left, and a healthy vasculature from a patient whose AMD is in remission on the right. The researchers developed an AI tool that allows ophthalmologists to glean the same information from photos that they would previously have needed to perform a biopsy to assess. Figures from a paper published in the journal Retina.
<関連情報>
- https://today.ucsd.edu/story/using-ai-to-enable-better-vision-for-both-humans-and-machines
- https://journals.lww.com/retinajournal/abstract/2024/03000/artificial_intelligence_for_optical_coherence.12.aspx
- https://journals.healio.com/doi/10.3928/23258160-20230130-03
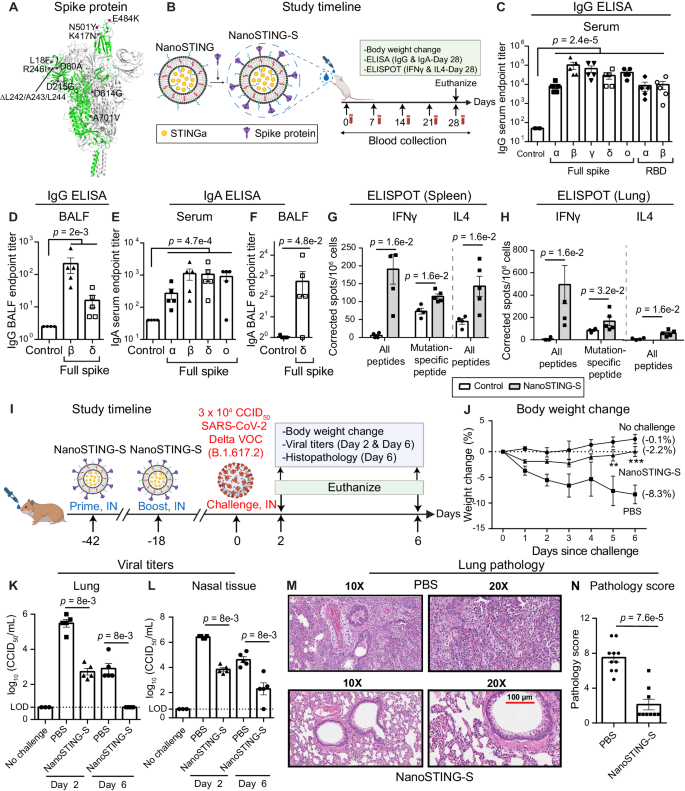
加齢黄斑変性における光干渉断層計アンギオグラフィーに基づく疾患活動性予測のための人工知能 ARTIFICIAL INTELLIGENCE FOR OPTICAL COHERENCE TOMOGRAPHY ANGIOGRAPHY–BASED DISEASE ACTIVITY PREDICTION IN AGE-RELATED MACULAR DEGENERATION
Heinke, Anna MD, PhD; Zhang, Haochen MS; Deussen, Daniel MD; Galang, Carlo Miguel B. MD; Warter, Alexandra MD; Kalaw, Fritz Gerald P. MD; Bartsch, Dirk-Uwe G. PhD; Cheng, Lingyun MD; An, Cheolhong PhD; Nguyen, Truong PhD; Freeman, William R. MD
Retina Published:March 2024
DOI: 10.1097/IAE.0000000000003977
Abstract
Purpose:
The authors hypothesize that optical coherence tomography angiography (OCTA)–visualized vascular morphology may be a predictor of choroidal neovascularization status in age-related macular degeneration (AMD). The authors thus evaluated the use of artificial intelligence (AI) to predict different stages of AMD disease based on OCTA en face 2D projections scans.
Methods:
Retrospective cross-sectional study based on collected 2D OCTA data from 310 high-resolution scans. Based on OCT B-scan fluid and clinical status, OCTA was classified as normal, dry AMD, wet AMD active, and wet AMD in remission with no signs of activity. Two human experts graded the same test set, and a consensus grading between two experts was used for the prediction of four categories.
Results:
The AI can achieve 80.36% accuracy on a four-category grading task with 2D OCTA projections. The sensitivity of prediction by AI was 0.7857 (active), 0.7142 (remission), 0.9286 (dry AMD), and 0.9286 (normal) and the specificity was 0.9524, 0.9524, 0.9286, and 0.9524, respectively. The sensitivity of prediction by human experts was 0.4286 active choroidal neovascularization, 0.2143 remission, 0.8571 dry AMD, and 0.8571 normal with specificity of 0.7619, 0.9286, 0.7857, and 0.9762, respectively. The overall AI classification prediction was significantly better than the human (odds ratio = 1.95, P = 0.0021).
Conclusion:
These data show that choroidal neovascularization morphology can be used to predict disease activity by AI; longitudinal studies are needed to better understand the evolution of choroidal neovascularization and features that predict reactivation. Future studies will be able to evaluate the additional predicative value of OCTA on top of other imaging characteristics (i.e., fluid location on OCT B scans) to help predict response to treatment.
並列画像と人工知能による重ね合わせ画像の精度と時間の比較 Accuracy and Time Comparison Between Side-by-Side and Artificial Intelligence Overlayed Images
Melina Cavichini, MD, MAS;Dirk-Uwe G. Bartsch, PhD;Alexandra Warter, MD;Sumit Singh, MD;Cheolhong An, PhD;Yiqian Wang, BS;Junkang Zhang, ME;Truong Nguyen, PhD; and William R. Freeman, MD
Ophthalmic Surgery, Lasers and Imaging Retina Published:February 01, 2023
DOI:https://doi.org/10.3928/23258160-20230130-03
Abstract
Background and Objective:
The purpose of this study was to evaluate the accuracy and the time to find a lesion, taken in different platforms, color fundus photographs and infrared scanning laser ophthalmoscope images, using the traditional side-by-side (SBS) colocalization technique to an artificial intelligence (AI)-assisted technique.
Patients and Methods:
Fifty-three pathological lesions were studied in 11 eyes. Images were aligned using SBS and AI overlaid methods. The location of each color fundus lesion on the corresponding infrared scanning laser ophthalmoscope image was analyzed twice, one time for each method, on different days, for two specialists, in random order. The outcomes for each method were measured and recorded by an independent observer.
Results:
The colocalization AI method was superior to the conventional in accuracy and time (P < .001), with a mean time to colocalize 37% faster. The error rate using AI was 0% compared with 18% in SBS measurements.
Conclusions:
AI permitted a more accurate and faster colocalization of pathologic lesions than the conventional method.