2025-01-24 コロンビア大学
<関連情報>
- https://www.engineering.columbia.edu/about/news/study-unveils-key-immune-cells-found-boost-cancer-treatment-success-acute-myeloid-leukemia
- https://www.science.org/doi/10.1126/sciimmunol.adr0782
白血病の骨髄微小環境における協調的免疫ネットワークが、細胞療法への反応を区別する Coordinated immune networks in leukemia bone marrow microenvironments distinguish response to cellular therapy
Katie Maurer, Cameron Y. Park, Shouvik Mani, Mehdi Borji, […], and Elham Azizi
Science Immunology Published:24 Jan 2025
DOI:https://doi.org/10.1126/sciimmunol.adr0782
Editor’s summary
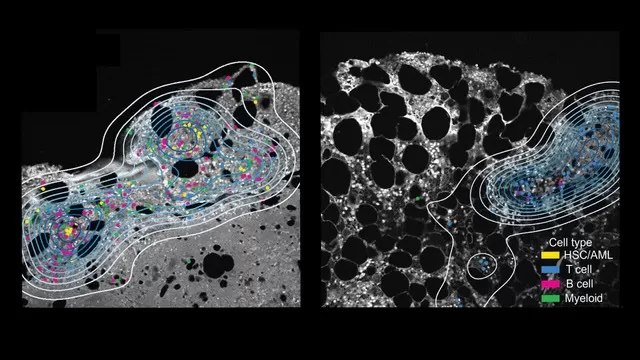
Hematopoietic stem cell transplantation (HSCT) represents the only potential cure for patients with aggressive myeloid leukemia. Donor lymphocyte infusion (DLI) is used to treat patients experiencing leukemia relapse after HSCT, but why some patients respond better to DLI immunotherapy remains unclear. Using single-cell and spatial transcriptomics, Maurer et al. analyzed longitudinal bone marrow samples from patients with relapsed acute myeloid leukemia (AML). Response to DLI was associated with expansion of ZNF683hi cytotoxic T cells, which were mostly derived from the DLI product and formed complex cellular networks with other bone marrow immune cells. Together, these findings provide insight into the features of effective antileukemia immune responses. —Claire Olingy
Abstract
Understanding how intratumoral immune populations coordinate antitumor responses after therapy can guide treatment prioritization. We systematically analyzed an established immunotherapy, donor lymphocyte infusion (DLI), by assessing 348,905 single-cell transcriptomes from 74 longitudinal bone marrow samples of 25 patients with relapsed leukemia; a subset was evaluated by both protein- and transcriptome-based spatial analysis. In acute myeloid leukemia (AML) DLI responders, we identified clonally expanded ZNF683+ CD8+ cytotoxic T lymphocytes with in vitro specificity for patient-matched AML. These cells originated primarily from the DLI product and appeared to coordinate antitumor immune responses through interaction with diverse immune cell types within the marrow microenvironment. Nonresponders lacked this cross-talk and had cytotoxic T lymphocytes with elevated TIGIT expression. Our study identifies recipient bone marrow microenvironment differences as a determinant of an effective antileukemia response and opens opportunities to modulate cellular therapy.