2025-02-11 バーミンガム大学
<関連情報>
- https://www.birmingham.ac.uk/news/2025/common-antibiotic-could-treat-inflammatory-bowel-disease-new-study-finds
- https://academic.oup.com/ecco-jcc/article/19/2/jjae189/7923930?login=false
原発性硬化性胆管炎-炎症性腸疾患におけるバンコマイシンの非盲検投与: 大腸疾患活動性の改善と宿主-微生物-メタボロームシグネチャーの変化との関連性 Open Label Vancomycin in Primary Sclerosing Cholangitis-Inflammatory Bowel Disease: Improved Colonic Disease Activity and Associations With Changes in Host–Microbiome–Metabolomic Signatures
Mohammed Nabil Quraishi, Jonathan Cheesbrough, Peter Rimmer, Benjamin H Mullish, Naveen Sharma, Elena Efstathiou, Animesh Acharjee, Georgios Gkoutus, Arzoo Patel, Julian R Marchesi …
Journal of Crohn’s and Colitis Published:14 December 2024
DOI:https://doi.org/10.1093/ecco-jcc/jjae189
Abstract
Background
We conducted a single-arm interventional study, to explore mucosal changes associated with clinical remission under oral vancomycin (OV) treatment, in primary sclerosing cholangitis-associated inflammatory bowel disease (PSC-IBD); NCT05376228.
Methods
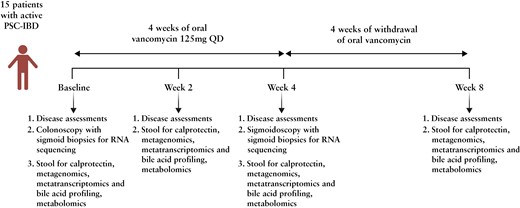
Fifteen patients with PSC and active colitis (median fecal calprotectin 459 µg/g; median total Mayo score 5) were treated with OV (125 mg QID) for 4 weeks and followed-up for a further 4 weeks of treatment withdrawal (8 weeks, end-of-study). Colonic biopsies were obtained at baseline and Week 4. Clinical assessments, and serum and stool samples (metagenomics, metatranscriptomics, and metabolomics) were collected at Weeks 0, 2, 4, and 8. The primary efficacy outcome measure was the induction of clinical remission.
Results
Oral vancomycin resulted in clinical remission in 12/15 patients and significant reductions in fecal calprotectin. Oral vancomycin was associated with reduced abundances of Lachnospiraceae, genera Blautia and Bacteroides; and enrichment of Enterobacteriaceae, and genera Veillonella, Akkermansia, and Escherichia. Oral vancomycin treatment was associated with the downregulation of multiple metatranscriptomic pathways (including short-chain fatty acid [SCFA] metabolism and bile acid [BA] biotransformation), along with host genes and multiple pathways involved in inflammatory responses and antimicrobial defence; and an upregulation of genes associated with extracellular matrix repair. Oral vancomycin use resulted in the loss of specific fecal SCFAs and secondary BAs, including lithocholic acid derivatives. Colitis activity relapsed following OV withdrawal, with host mucosal and microbial changes trending toward baseline.
Conclusions
Four weeks of OV induces remission in PSC-IBD activity, associated with a reduction in gut bacterial diversity and compositional changes relating to BA and SCFA homeostasis.

