2025-02-25 カロリンスカ研究所(KI)
<関連情報>
- https://news.ki.se/antidepressants-linked-to-faster-cognitive-decline-in-dementia
- https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03851-3
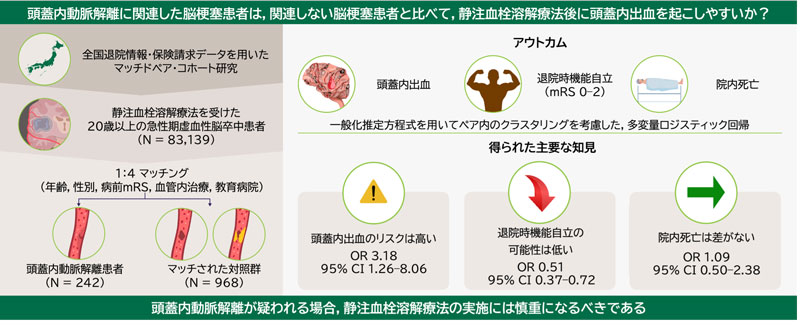
認知症患者における抗うつ薬の使用と認知機能の低下:全国コホート研究 Antidepressant use and cognitive decline in patients with dementia: a national cohort study
Minjia Mo,Tamar Abzhandadze,Minh Tuan Hoang,Simona Sacuiu,Pol Grau Jurado,Joana B. Pereira,Luana Naia,Julianna Kele,Silvia Maioli,Hong Xu,Maria Eriksdotter & Sara Garcia-Ptacek
BMC Medicine Published:25 February 2025
DOI:https://doi.org/10.1186/s12916-025-03851-3
Abstract
Background
Dementia is associated with psychiatric symptoms but the effects of antidepressants on cognitive function in dementia are understudied. We aimed to investigate the association between antidepressants and cognitive decline in patients with dementia, and the risk of severe dementia, fractures and death, depending on antidepressant class, drug, and dose.
Methods
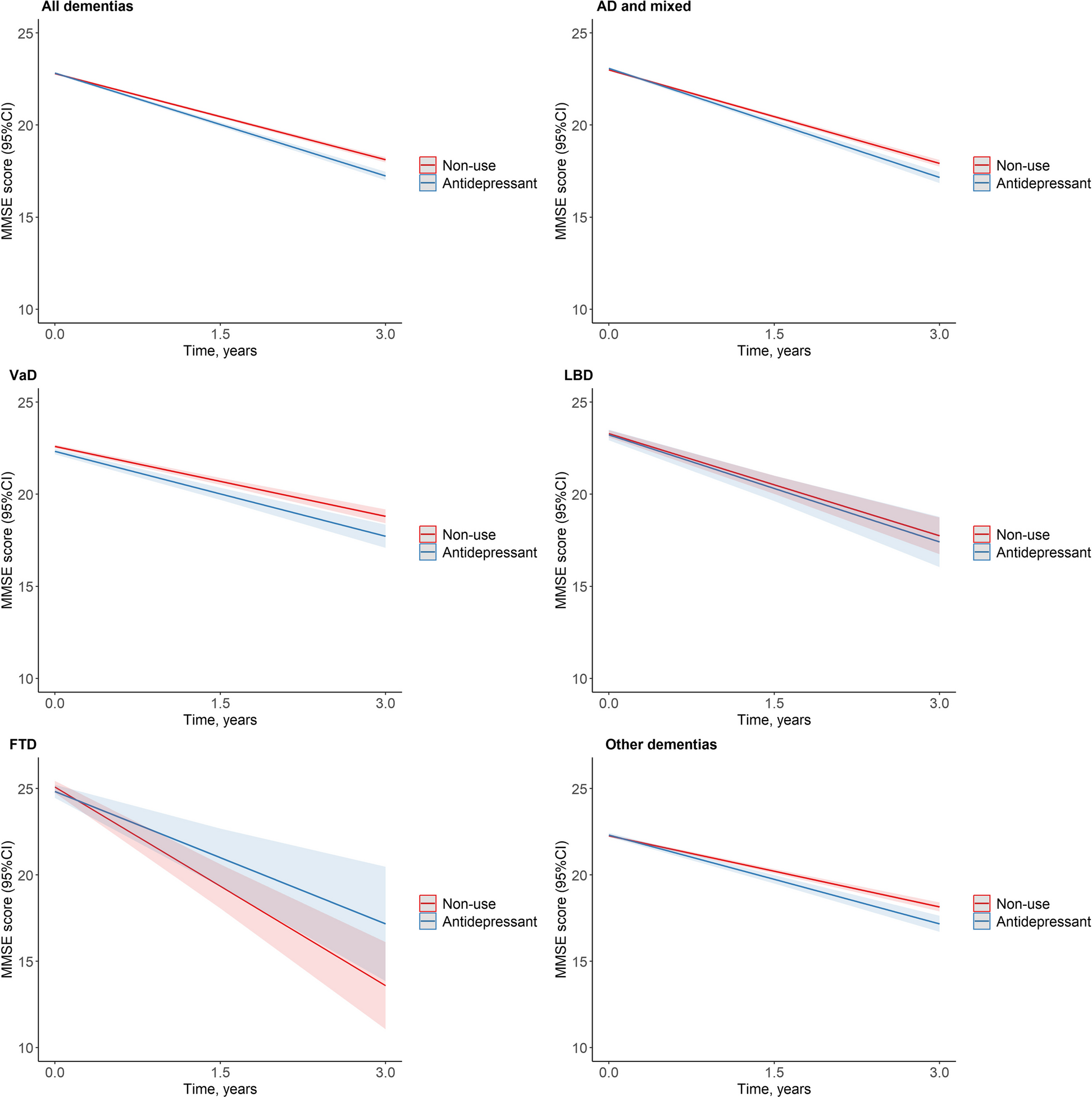
This is a national cohort study. Patients with dementia registered in the Swedish Registry for Cognitive/Dementia Disorders-SveDem from May 1, 2007, until October 16, 2018, with at least one follow-up after dementia diagnosis, and who were new users of antidepressants, were included. Antidepressant use as a time varying exposure defined during the 6 months leading up to dementia diagnosis or each subsequent follow-up. We used linear mixed models to examine the association between antidepressant use and cognitive trajectories assessed by Mini-Mental State Examination (MMSE) scores. We used Cox proportional hazards models to calculate the hazard ratios for severe dementia (MMSE score < 10), fracture, and death. We compared antidepressant classes and drugs, and analyzed dose–response.
Results
We included 18740 patients (10 205 women [54.5%]; mean [SD] age, 78.2[7.4] years), of which 4271 (22.8%) received at least one prescription for an antidepressant. During follow-up, a total of 11912 prescriptions for antidepressants were issued, with selective serotonin reuptake inhibitors (SSRI) being the most common (64.8%). Antidepressant use was associated with faster cognitive decline (β (95% CI) = - 0.30(- 0.39, - 0.21) points/year), in particular sertraline (- 0.25(- 0.43, - 0.06) points/year), citalopram (- 0.41(- 0.55, - 0.27) points/year), escitalopram (- 0.76(- 1.09, - 0.44) points/year), and mirtazapine (- 0.19(- 0.34, - 0.04) points/year) compared with non-use. The association was stronger in patients with severe dementia (initial MMSE scores 0–9). Escitalopram showed a greater decline rate than sertraline. Compared with non-use, dose response of SSRIs on greater cognitive decline and higher risks of severe dementia, all-cause mortality, and fracture were observed.
Conclusions
In this cohort study, current antidepressant use was associated with faster cognitive decline; furthermore, higher dispensed doses of SSRIs were associated with higher risk for severe dementia, fractures, and all-cause mortality. These findings highlight the significance of careful and regular monitoring to assess the risks and benefits of different antidepressants use in patients with dementia.