2025-04-23 ジョンズ・ホプキンス大学(JHU)
<関連情報>
- https://hub.jhu.edu/2025/04/23/nsf-funding-suchia-saria-sepsis-detection/
- https://www.nature.com/articles/s41591-022-01895-z
TREWS機械学習ベースの早期警告システムのプロバイダー採用を促進する要因と敗血症治療タイミングへの影響 Factors driving provider adoption of the TREWS machine learning-based early warning system and its effects on sepsis treatment timing
Katharine E. Henry,Roy Adams,Cassandra Parent,Hossein Soleimani,Anirudh Sridharan,Lauren Johnson,David N. Hager,Sara E. Cosgrove,Andrew Markowski,Eili Y. Klein,Edward S. Chen,Mustapha O. Saheed,Maureen Henley,Sheila Miranda,Katrina Houston,Robert C. Linton II,Anushree R. Ahluwalia,Albert W. Wu & Suchi Saria
Nature Medicine Published:21 July 2022
DOI:https://doi.org/10.1038/s41591-022-01895-z
Abstract
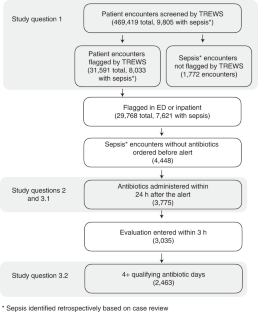
Machine learning-based clinical decision support tools for sepsis create opportunities to identify at-risk patients and initiate treatments at early time points, which is critical for improving sepsis outcomes. In view of the increasing use of such systems, better understanding of how they are adopted and used by healthcare providers is needed. Here, we analyzed provider interactions with a sepsis early detection tool (Targeted Real-time Early Warning System), which was deployed at five hospitals over a 2-year period. Among 9,805 retrospectively identified sepsis cases, the early detection tool achieved high sensitivity (82% of sepsis cases were identified) and a high rate of adoption: 89% of all alerts by the system were evaluated by a physician or advanced practice provider and 38% of evaluated alerts were confirmed by a provider. Adjusting for patient presentation and severity, patients with sepsis whose alert was confirmed by a provider within 3 h had a 1.85-h (95% CI 1.66–2.00) reduction in median time to first antibiotic order compared to patients with sepsis whose alert was either dismissed, confirmed more than 3 h after the alert or never addressed in the system. Finally, we found that emergency department providers and providers who had previous interactions with an alert were more likely to interact with alerts, as well as to confirm alerts on retrospectively identified patients with sepsis. Beyond efforts to improve the performance of early warning systems, efforts to improve adoption are essential to their clinical impact and should focus on understanding providers’ knowledge of, experience with and attitudes toward such systems.


