2025-05-01 アメリカ国立衛生研究所(NIH)
<関連情報>
- https://www.nih.gov/news-events/news-releases/many-genes-male-female-placentas-expressed-differently
- https://www.nature.com/articles/s41467-025-58128-3
- https://jamanetwork.com/journals/jamapediatrics/fullarticle/2661822
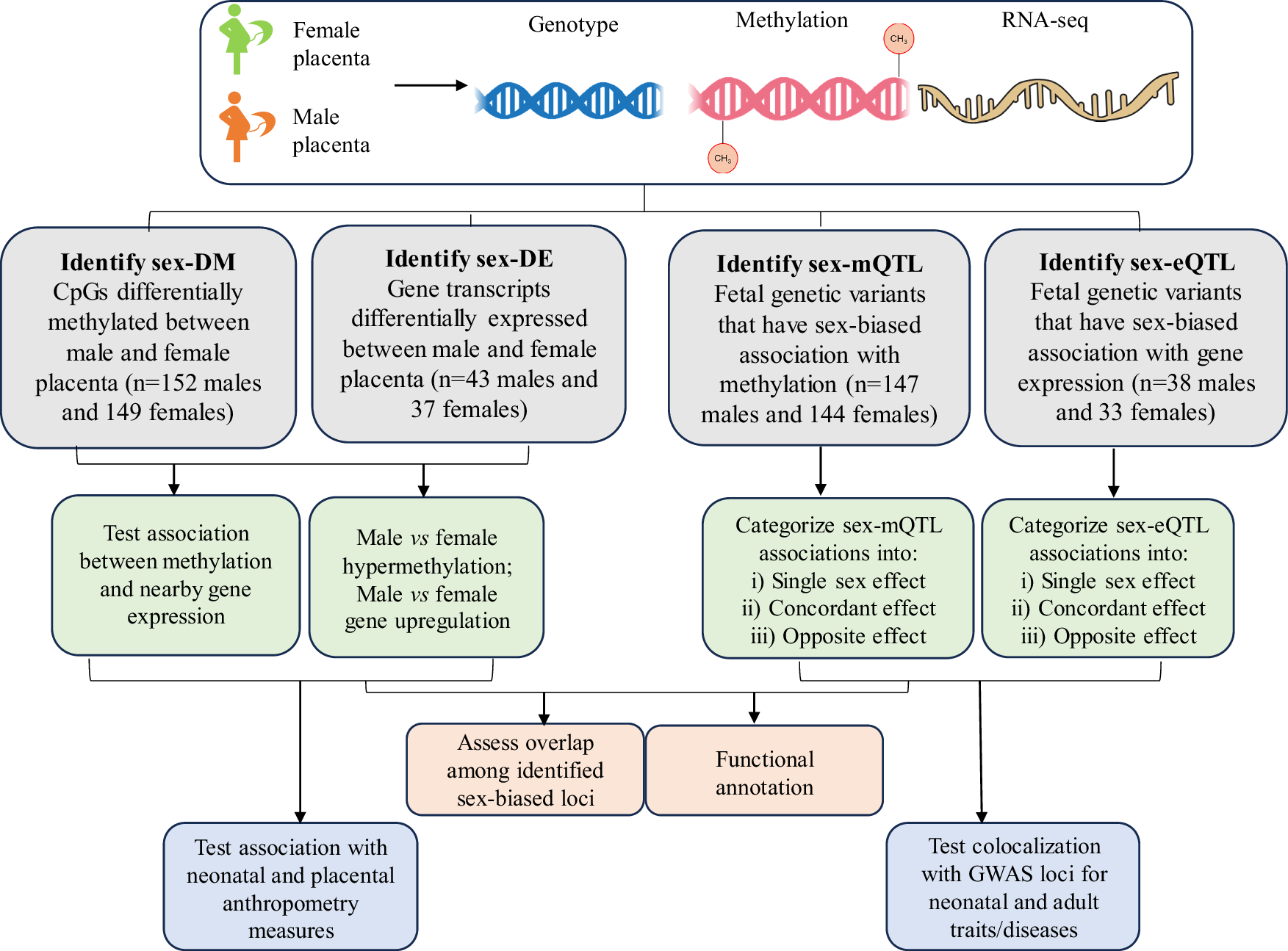
胎盤の性分化に伴うメチル化と遺伝子発現制御が新生児形質や成人病に関与していることが明らかになった Sex-differentiated placental methylation and gene expression regulation has implications for neonatal traits and adult diseases
Fasil Tekola-Ayele,Richard J. Biedrzycki,Tesfa Dejenie Habtewold,Prabhavi Wijesiriwardhana,Amber Burt,Carmen J. Marsit,Marion Ouidir & Ronald Wapner
Nature Communications Published:01 May 2025
DOI:https://doi.org/10.1038/s41467-025-58128-3
Abstract
Sex differences in physiological and disease traits are pervasive and begin during early development, but the genetic architecture of these differences is largely unknown. Here, we leverage the human placenta, a transient organ during pregnancy critical to fetal development, to investigate the impact of sex in the regulatory landscape of placental autosomal methylome and transcriptome, and its relevance to health and disease. We find that placental methylation and its genetic regulation are extensively impacted by fetal sex, whereas sex differences in placental gene expression and its genetic regulation are limited. We identify molecular processes and regulatory targets that are enriched in a sex-specific manner, and find enrichment of imprinted genes in sex-differentiated placental methylation, including female-biased methylation within the well-known KCNQ1OT1/CDKN1C imprinting cluster of genes expressed in a parent-of-origin dependent manner. We establish that several sex-differentiated genetic effects on placental methylation and gene expression colocalize with birthweight and adult disease genetic associations, facilitating mechanistic insights on early life origins of health and disease outcomes shaped by sex.
母親の肥満と胎児成長の縦断的超音波測定との関連性 NICHD胎児発育研究-Singletonsからの所見 Association of Maternal Obesity With Longitudinal Ultrasonographic Measures of Fetal Growth Findings From the NICHD Fetal Growth Studies–Singletons
Cuilin Zhang, MD, MPH, PhD; Mary L. Hediger, PhD; Paul S. Albert, PhD; et al
JAMA Pediatrics Published:January 2018
DOI:10.1001/jamapediatrics.2017.3785
Key Points
Question What are the associations of maternal obesity with fetal growth, and when do these associations start emerging?
Findings In a longitudinal cohort study that included 468 obese and 2334 nonobese pregnant women, the femur length, humerus length, head circumference, and estimated weight of fetuses were significantly greater in the fetuses of obese women compared with fetuses of nonobese women. Differences commenced as early as 21 weeks’ gestation.
Meaning Fetal growth differs in obese and nonobese pregnant women; the mechanisms of these findings and their long-term implications for child and adult health remain to be established.
Abstract
Importance Despite the increasing prevalence of pregravid obesity, systematic evaluation of the association of maternal obesity with fetal growth trajectories is lacking.
Objective To characterize differences in fetal growth trajectories between obese and nonobese pregnant women, and to identify the timing of any observed differences.
Design, Setting, and Participants The Eunice Kennedy Shriver National Institute of Child Health and Human Development Fetal Growth Studies–Singletons study enrolled cohorts of pregnant women at 12 US health care institutions. Obese women (with prepregnancy body mass index > 30) and nonobese women (prepregnancy body mass indexes, 19-29.9) without major chronic diseases were recruited between 8 weeks and 0 days’ gestation and 13 weeks and 6 days’ gestation. A mixed longitudinal randomization scheme randomized participants into 1 of 4 schedules for 2-dimensional and 3-dimensional ultrasonograms to capture weekly fetal growth data throughout the remainder of their pregnancies.
Main Outcomes and Measures On each ultrasonogram, fetal humerus length, femur length, biparietal diameter, head circumference, and abdominal circumference were measured. Fetal growth curves were estimated using linear mixed models with cubic splines. Median differences in the fetal measures at each gestational week of the obese and nonobese participants were examined using the likelihood ratio and Wald tests after adjustment for maternal characteristics.
Results The study enrolled 468 obese and 2334 nonobese women between 8 weeks and 0 days’ gestation and 13 weeks and 6 days’ gestation. After a priori exclusion criteria, 443 obese and 2320 nonobese women composed the final cohort. Commencing at 21 weeks’ gestation, femur length and humerus length were significantly longer for fetuses of obese woman than those of nonobese women. Differences persisted in obese and nonobese groups through 38 weeks’ gestation (median femur length, 71.0 vs 70.2 mm; P = .01; median humerus length, 62.2 vs 61.6 mm; P = .03). Averaged across gestation, head circumference was significantly larger in fetuses of obese women than those of nonobese women (P = .02). Fetal abdominal circumference was not greater in the obese cohort than in the nonobese cohort but was significantly larger than in fetuses of normal-weight women (with body mass indexes between 19.0-24.9) commencing at 32 weeks (median, 282.1 vs 280.2 mm; P = .04). Starting from 30 weeks’ gestation, estimated fetal weight was significantly larger for the fetuses of obese women (median, 1512 g [95% CI, 1494-1530 g] vs 1492 g [95% CI, 1484-1499 g]) and the difference grew as gestational age increased. Birth weight was higher by almost 100 g in neonates born to obese women than to nonobese women (mean, 3373.2 vs 3279.5 g).
Conclusions and Relevance As early as 32 weeks’ gestation, fetuses of obese women had higher weights than fetuses of nonobese women. The mechanisms and long-term health implications of these findings are not yet established.