2025-05-09 カロリンスカ研究所(KI)
<関連情報>
- https://news.ki.se/fatty-liver-in-pregnancy-may-increase-risk-of-preterm-birth
- https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(25)00170-1/fulltext
生検で証明されたMASLD女性における妊娠・出産の有害転帰:全国規模のコホート研究 Adverse pregnancy and birth outcomes in women with biopsy-proven MASLD: a nationwide cohort study
Carole A. Marxer ∙ Fahim Ebrahimi ∙ David Bergman ∙ Jiangwei Sun ∙ Hannes Hagström ∙ Marcus Thuresson ∙ et al.
eClinicalMedicine Published: May 9, 2025
DOI:https://doi.org/10.1016/j.eclinm.2025.103238
Summary
Background
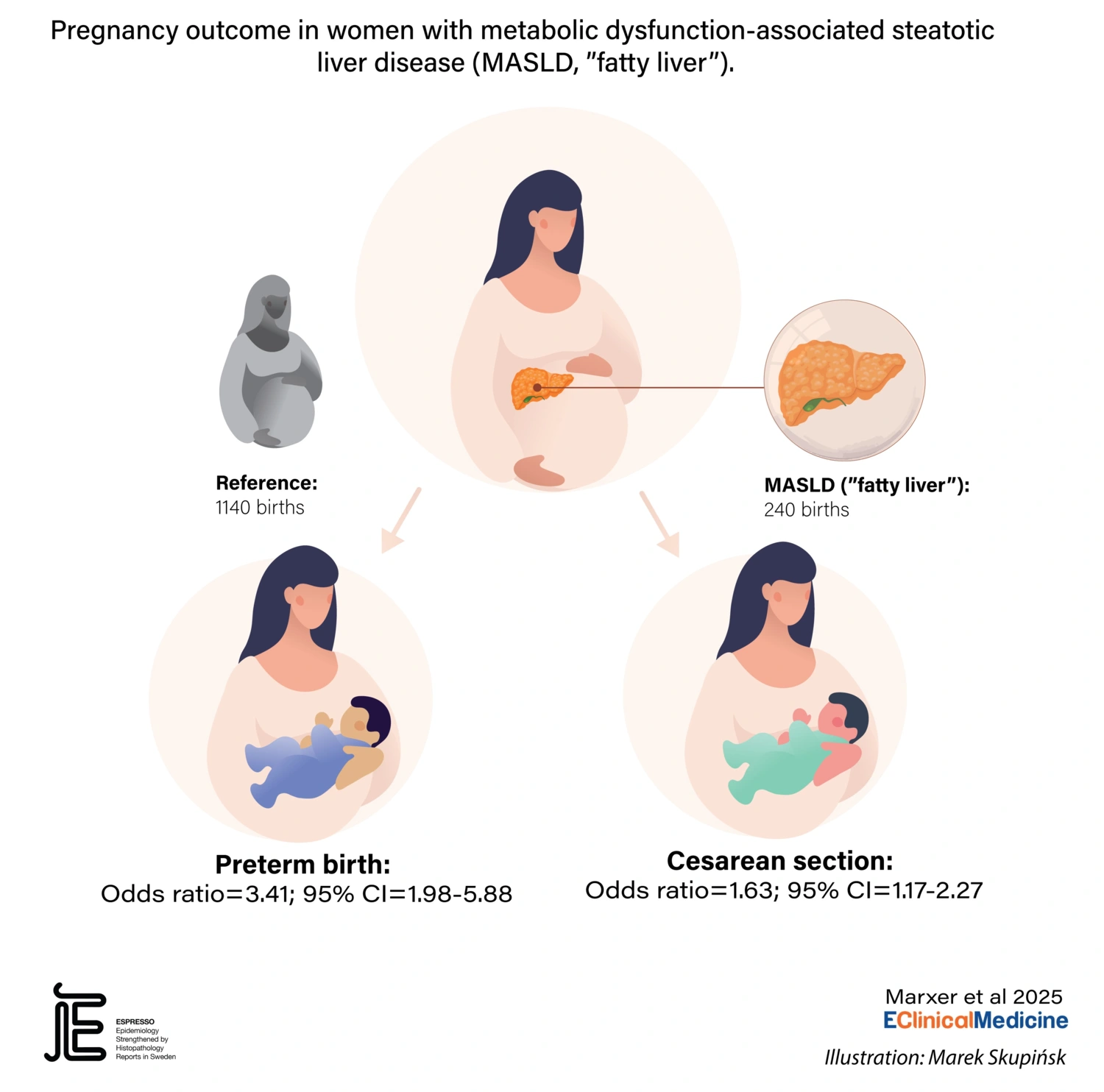
Metabolic dysfunction-associated steatotic liver disease (MASLD) has been linked to an increased risk of adverse pregnancy outcomes. We aimed to assess the roles of obesity, familial factors, and disease severity.
Methods
Nationwide cohort study in Sweden (1992–2017) including 240 births (162 women) with biopsy-proven MASLD vs. 1140 matched reference births (1138 women). Multivariable conditional logistic regression determined adjusted odds ratios (aORs) for adverse pregnancy outcomes.
Findings
Preterm birth occurred in 40 (16.7%) births of women with MASLD compared to 53 (4.7%) in reference births, yielding an aOR of 3.41 (95% CI = 1.98–5.88), which remained increased when compared with overweight/obese women without known MASLD (aOR = 4.60, 95% CI = 2.00–10.60). The association was observed for both medically indicated preterm birth (aOR = 11.90, 95% CI = 2.46–57.59) and spontaneous preterm birth (aOR = 2.42, 95% CI = 1.16–5.04). The aOR of preterm birth did not increase with MASLD severity (MASH without fibrosis/noncirrhotic fibrosis/cirrhosis: aOR = 1.53, 95% CI = 0.23–10.02), but 95% CIs were wide. MASLD was linked to increased odds of cesarean section (aOR = 1.63, 95% CI = 1.17–2.27), but not when compared with overweight/obese reference women (aOR = 1.20, 95% CI = 0.77–1.86). Our results indicate comparable Apgar scores, and similar rates of congenital malformation, stillbirth and neonatal death in both groups. Main results were confirmed in sibling analyses (i.e., when comparing to births of full female siblings of the mothers).
Interpretation
MASLD is a risk factor for preterm birth, independent of obesity and familial factors. MASLD however does not indicate more stillbirths and neonatal deaths. We did not find more adverse pregnancy outcomes with increasing MASLD severity.
Funding
Swiss National Science Foundation (P500PM_217670, P500PM_210866), European Crohn’s and Colitis Organisation and, The Swedish Society for Medical Research (PG-23-0315-H-02) and Karolinska Institute.