2025-05-13 英国研究イノベーション機構(UKRI)
<関連情報>
- https://www.ukri.org/news/multiple-chronic-illnesses-linked-to-higher-risk-of-depression/
- https://www.nature.com/articles/s43856-025-00825-7
英国バイオバンクデータのクラスターおよび生存分析により、身体的多疾患クラスターとその後のうつ病との関連が明らかになった Cluster and survival analysis of UK biobank data reveals associations between physical multimorbidity clusters and subsequent depression
Lauren Nicole DeLong,Kelly Fleetwood,Regina Prigge,Paola Galdi,Bruce Guthrie & Jacques D. Fleuriot
Communications Medicine Published:13 May 2025
DOI:https://doi.org/10.1038/s43856-025-00825-7
Abstract
Background
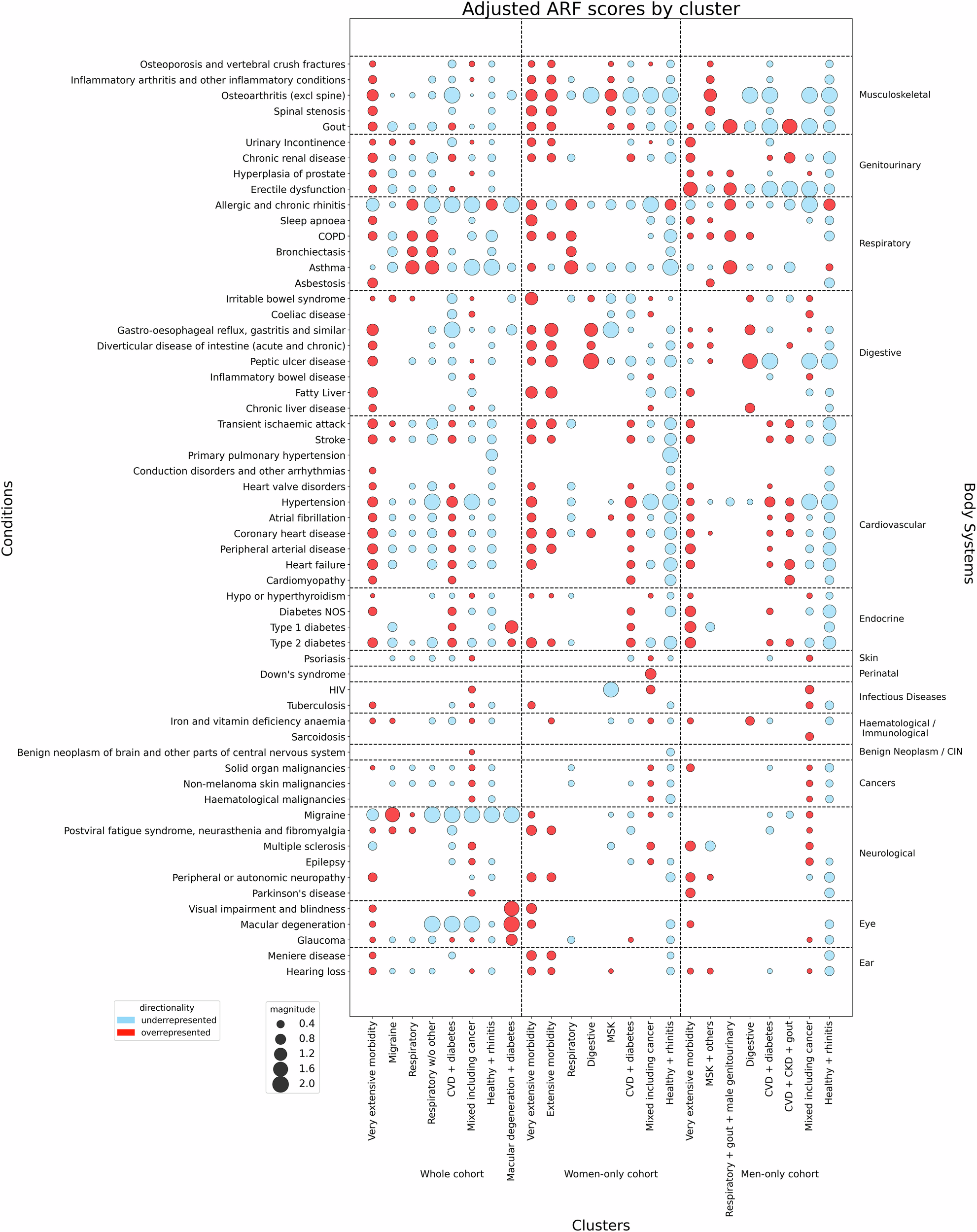
Multimorbidity, the co-occurrence of two or more conditions within an individual, is a growing challenge for health and care delivery as well as for research. Combinations of physical and mental health conditions are highlighted as particularly important. Here, we investigated associations between physical multimorbidity and subsequent depression.
Methods
We performed a clustering analysis upon physical morbidity data for UK Biobank participants aged 37–73. Of 502,353 participants, 142,005 had linked general practice data with at least one baseline physical condition. Following stratification by sex (77,785 women; 64,220 men), we used four clustering methods and selected the best-performing based on clustering metrics. We used Fisher’s Exact test to determine significant over-/under-representation of conditions within each cluster. Amongst people with no prior depression, we used survival analysis to estimate associations between cluster-membership and time to subsequent depression diagnosis.
Results
Our results show that the k-modes models perform best, and the over-/under-represented conditions in the resultant clusters reflect known associations. For example, clusters containing an overrepresentation of cardiometabolic conditions are amongst the largest (15.5% of whole cohort, 19.7% of women, 24.2% of men). Cluster associations with depression vary from hazard ratio 1.29 (95% confidence interval 0.85–1.98) to 2.67 (2.24–3.17), but almost all clusters show a higher association with depression than those without physical conditions.
Conclusions
We show that certain groups of physical multimorbidity may be associated with a higher risk of subsequent depression. However, our findings invite further investigation into other factors, such as social considerations, which may link physical multimorbidity with depression.
Plain language summary
Multimorbidity occurs when an individual has two or more diseases. Previous multimorbidity research often focused on physical disease, but the links between physical and mental health are increasingly recognised as important. Here, we investigate whether certain patterns of physical conditions affect the risk of developing depression. To do so, we use computational methods to identify groups of physical diseases that co-occur. We identify several groups and then explore whether participants in each group were diagnosed with depression. Although risk of depression varies across groups, we show that those with physical diseases have a higher risk than those without. We recommend further studies to investigate other factors which may link physical disease to depression.