2025-05-05 カリフォルニア大学ロサンゼルス校(UCLA)
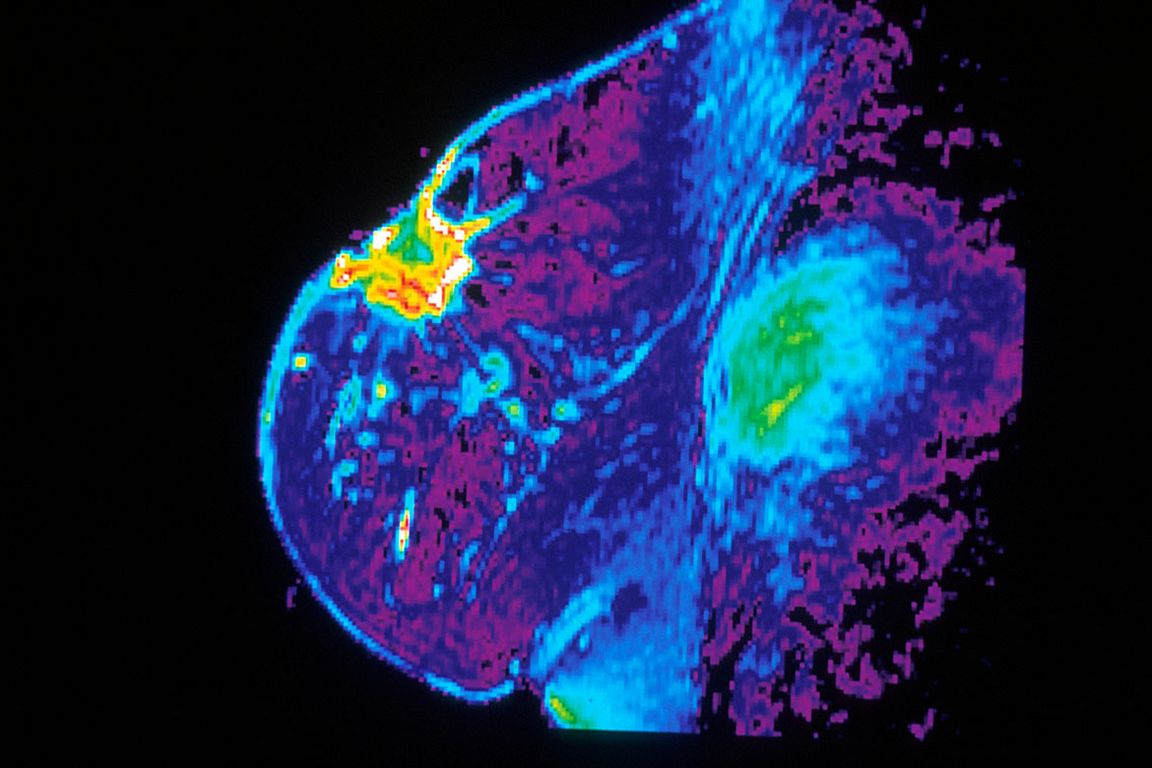
Dr. Steven Harmes/Cancer.Gov
<関連情報>
- https://newsroom.ucla.edu/releases/ai-early-detection-breast-cancers-ucla-study
- https://academic.oup.com/jnci/advance-article/doi/10.1093/jnci/djaf103/8116029
乳癌のマンモグラフィ分類と人工知能の性能 Mammographic classification of interval breast cancers and artificial intelligence performance
Tiffany T Yu, MD , Anne C Hoyt, MD , Melissa M Joines, MD , Cheryce P Fischer, MD , Nazanin Yaghmai, MD , James S Chalfant, MD , Lucy Chow, MD , Shabnam Mortazavi, MD , Christopher D Sears, BS , James Sayre, PhD…
JNCI: Journal of the National Cancer Institute Published:18 April 2025
DOI:https://doi.org/10.1093/jnci/djaf103
Abstract
Background
European studies suggest artificial intelligence (AI) can reduce interval breast cancers (IBCs). However, research on IBC classification and AI’s effectiveness in the U.S., particularly using digital breast tomosynthesis (DBT) and annual screening, is limited. We aimed to mammographically classify IBCs and assess AI performance using a 12-month screening interval.
Methods
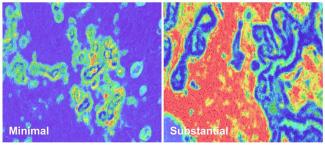
From digital mammography (DM) and DBT screening mammograms acquired 2010-2019 at a U.S. tertiary care academic center, we identified IBCs diagnosed <12 months after a negative mammogram. At least three breast radiologists retrospectively classified IBCs as missed-reading error, minimal signs-actionable, minimal signs-non-actionable, true interval, occult, or missed-technical error. A deep-learning AI tool assigned risk scores (1-10) to the negative index screening mammograms, with scores ≥8 considered “flagged.” Statistical analysis evaluated associations among IBC types and AI exam scores, AI markings, and patient/tumor characteristics.
Results
From 184,935 screening mammograms (65% DM, 35% DBT), we identified 148 IBCs in 148 women (mean age, 61±12 years). Of these, 26% were minimal signs-actionable; 24% occult; 22% minimal signs-non-actionable; 17% missed-reading error; 6% true interval; and 5% missed-technical error (p<.001). AI scored 131 mammograms (17 errors excluded). AI most frequently flagged exams with missed-reading errors (90%), minimal signs-actionable (89%) and minimal signs-non-actionable (72%) (p=.02). AI localized mammographically-visible types more accurately (35-68%) than non-visible types (0-50%, p=.02).
Conclusion
AI more frequently flagged and accurately localized IBC types that were mammographically visible at screening (missed or minimal signs), as compared to true interval or occult cancers.