2025-06-10 カロリンスカ研究所(KI)
<関連情報>
- https://news.ki.se/newborns-with-health-problems-are-at-higher-risk-of-dying-into-adolescence
- https://jamanetwork.com/journals/jamapediatrics/fullarticle/2835130
新生児期の重症罹患率と乳児期および青年期後期までの全死因死亡率および原因別死亡率 Severe Neonatal Morbidity and All-Cause and Cause-Specific Mortality Through Infancy and Late Adolescence
Hillary Graham, MS; Kari Johansson, PhD; Martina Persson, MD, PhD; et al
JAMA Pediatrics Published:June 10, 2025
DOI:10.1001/jamapediatrics.2025.1873
Key Points
Question Is a severe neonatal morbidity (SNM) diagnosis during the first 27 postnatal days associated with later mortality after surviving the neonatal period?
Findings In this cohort study of 2 million live-born singleton infants, 49 225 (2.4%) were diagnosed with SNM. Children with SNM had higher rate of postneonatal death than those without SNM.
Meaning These findings suggest that SNM is associated with an increased risk of childhood mortality.
Abstract
Importance Severe neonatal morbidity (SNM) has been associated with neonatal and early life mortality, yet its longer-term associations and cause-specific mortality remain unknown.
Objectives To examine the association between SNM during the first 27 postnatal days and all-cause and cause-specific mortality from infancy through late adolescence.
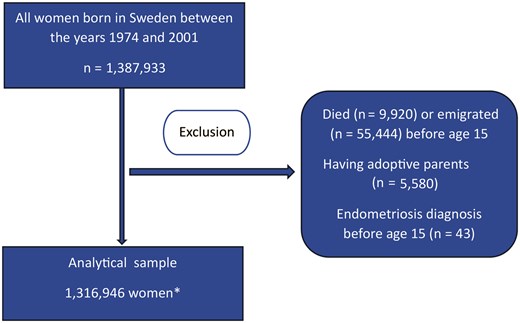
Design, Setting, and Participants This population-based cohort study was conducted in Sweden and involved 2 098 752 live-born singleton neonates with 22 or more weeks’ gestation, born between January 2002 and December 2021, who survived and did not emigrate during the neonatal period. Mortality data were collected through March 2023, and data analysis was performed from July 2024 to December 2024.
Exposures Neonates with any SNM diagnoses or procedures within 27 days after birth.
Main Outcomes and Measures The primary outcomes were all-cause mortality and cause-specific mortality from 28 days up to a maximum of 21.2 years. Adjusted hazard ratios (aHRs) and 95% confidence intervals were estimated using Cox proportional hazards models and adjusted for infant and maternal characteristics. A sibling-control analysis was also performed.
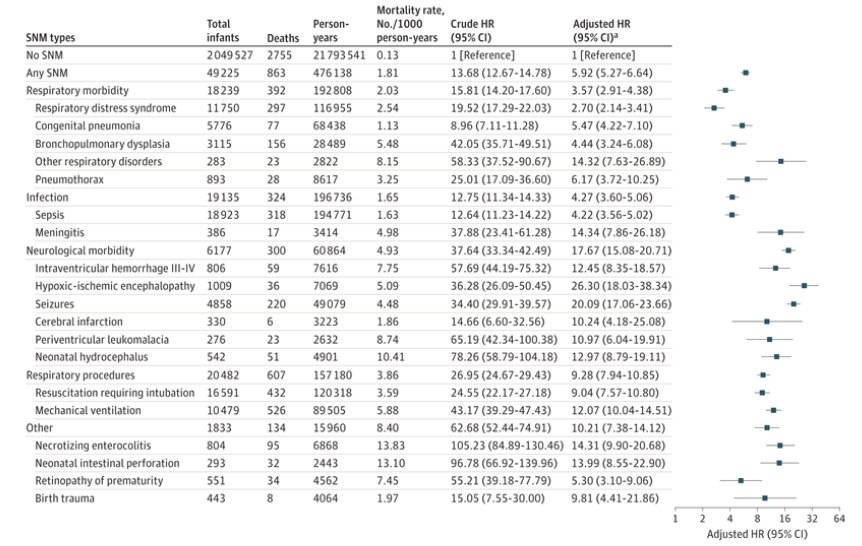
Results Among 2 098 752 children included in the study, 49 225 children (2.4%) were diagnosed with SNM during the neonatal period. During the median (IQR) follow-up duration of 10.5 (5.7-15.6) years, overall 3618 children died. The mortality rate for children with SNM was 1.81 per 1000 person-years compared with a rate of 0.13 per 1000 person-years for those without SNM, with an aHR of 5.92 (95% CI, 5.27-6.64). Neonatal neurological conditions were the leading morbidity, associated with a 17.67-fold increase in all-cause mortality after 28 days of life (95% CI, 15.08-20.71). The aHRs for the association between SNM and all-cause mortality were higher in female children than in male children and in those born at term. SNM was associated with elevated mortality risk from infections and disorders in the nervous, circulatory, respiratory, and metabolic systems until the earliest date of death, censoring due to emigration, or the end of follow-up. Sibling-control analysis showed the associations were unaffected by familial confounding.
Conclusions and Relevance Findings from this cohort study suggest that SNM may be a significant risk factor for childhood mortality. Efforts to prevent SNM, as well as early identification and long-term follow-up care, may help further reduce mortality.