2025-09-02 オックスフォード大学
<関連情報>
- https://www.ox.ac.uk/news/2025-09-02-teenage-period-pain-linked-higher-risk-chronic-pain-adulthood
- https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(25)00213-5/fulltext
思春期月経困難症と成人期慢性疼痛の縦断的関連性:英国人口ベース研究 Longitudinal association between dysmenorrhoea in adolescence and chronic pain in adulthood: a UK population-based study
Rachel Reid-McCann, PhD ∙ Prof Omero B Poli-Neto, PhD ∙ Kate Stein, MBBS ∙ Sharon Dixon, MBBS ∙ Emma Cox, MBA ∙ Lydia Coxon, DPhil ∙ et al.
The Lancet Child & Adolescent Health Published: August 31, 2025
DOI:https://doi.org/10.1016/S2352-4642(25)00213-5
00213-5/asset/b1687a8a-87b6-4c93-8371-fbaf48cc56d0/main.assets/gr1.jpg)
Summary
Background
Dysmenorrhoea affects many adolescents and often goes untreated for various sociocultural reasons. Dysmenorrhoea frequently co-occurs with other chronic pain conditions, and adult women with dysmenorrhoea have greater sensory sensitivity compared with controls. We aimed to test the hypothesis that adolescent dysmenorrhoea leads to the development of general chronic pain, including pain outside the pelvis, by estimating the risk of chronic pain in adulthood following the experience of dysmenorrhoea at age 15 years.
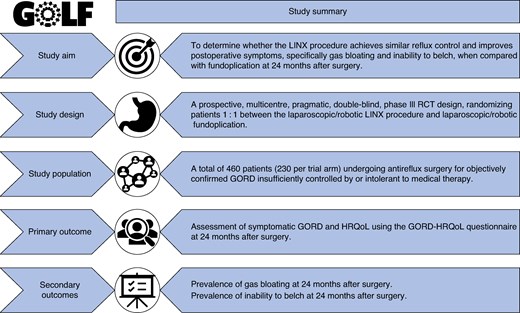
Methods
We used data from the Avon Longitudinal Study of Parents and Children (ALSPAC) a longitudinal birth cohort of mothers with an expected delivery date between April 1, 1991, and Dec 31, 1992, and their children in Avon, UK. Each year from ages 8 to 17 years, children were asked about dysmenorrhoea. At age 15, participants were also asked to describe their experience of dysmenorrhea as mild, moderate, or severe. At age 26 years, participants reported any pain in response to the questions: “Have you had any aches or pains that have lasted for a day or longer in the past month?” (yes or no); and “When did the pain start?” (<3 months ago or ≥3 months ago). Any chronic pain (≥3 months in duration) was the primary outcome. For the analysis, we excluded participants with a pain condition before menarche and participants with acute pain lasting less than 3 months at age 26 years. Missing data were addressed by multiple imputation. To estimate the risk of chronic pain at age 26 years when experiencing dysmenorrhoea in adolescence (none, mild, moderate, or severe), we used multivariable logistic regression models, adjusted for confounders previously associated with dysmenorrhoea and chronic pain (ethnicity, mother’s education level, adverse childhood experiences from ages 0–10 years, depressive symptoms preceding menarche, frequency of vigorous physical activity at menarche, smoking at menarche, polyunsaturated fatty acid intake as per food diaries completed at age 10 years, and BMI at menarche), to generate relative risks [RRs] for chronic pain. Dose response was investigated in an adjusted regression model with dysmenorrhoea severity as a numeric variable. We examined anxiety and depressive symptoms in the 2 years after dysmenorrhoea was reported as potential mediators using bootstrapping with 1000 simulations.
Findings
The study sample included 1157 participants, 691 (59·7%) of whom reported moderate or severe dysmenorrhoea at age 15 years. Of the 307 (26·5%) participants who reported chronic pain at age 26 years, 32 (17·3%) had no dysmenorrhoea at age 15 whereas 62 (22·1%) had mild, 157 (30·0%) had moderate, and 56 (33·5%) had severe dysmenorrhoea. Adjusted RRs for any chronic pain at age 26 years were 1·23 (95% CI 0·85–1·74, p=0·27) for mild, 1·65 (1·22–2·18, p=0·0021) for moderate, and 1·76 (1·23–2·39, p=0·0030) for severe dysmenorrhoea at age 15 years compared with no dysmenorrhoea. These findings correspond to an absolute adjusted risk difference of 4·8 percentage points (95% CI –2·5 to 12·1) for mild dysmenorrhoea, 12·7 percentage points (5·9 to 19·4) for moderate dysmenorrhoea, and 16·2 percentage points (7·2 to 25·2) for severe dysmenorrhoea compared with no dysmenorrhea. Anxiety and depressive symptoms mediated a small proportion of the association between severe dysmenorrhoea and chronic pain. The mediating role of anxiety and depressive symptoms was greatest among participants with severe dysmenorrhoea.
Interpretation
Dysmenorrhoea in adolescence adversely affects immediate wellbeing and contributes to an increased risk of chronic pain in adulthood, thus lending supporting evidence to calls to consider adolescent dysmenorrhoea a crucial public health issue. Future work should focus on early identification and effective management, including non-pharmacological strategies and self-management, which relies on continuing work to improve young people’s menstrual literacy.
Funding
UK Research and Innovation Strategic Priorities Fund Advanced Pain Discovery Platform, a co-funded initiative by UK Research and Innovation (UK Medical Research Council, Biotechnology and Biological Sciences Research Council, and Economic and Social Research Council), Versus Arthritis, the Medical Research Foundation, and Eli Lilly and Company.