2025-09-10 カリフォルニア大学サンタバーバラ校(UCSB)
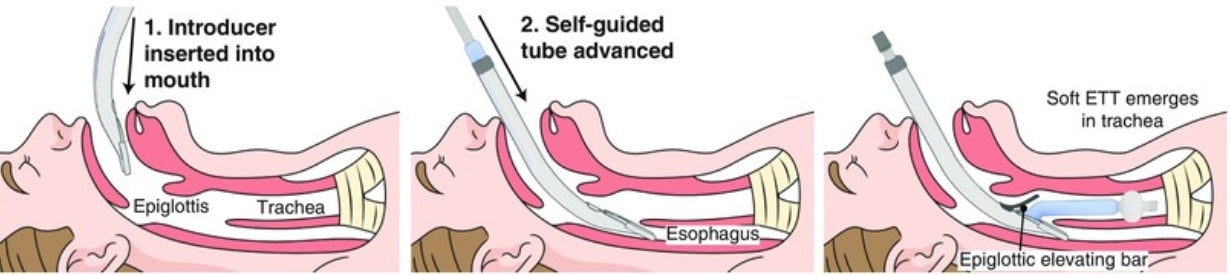
Photo Credit:Courtesy Image
An illustration of how the intubation device is used
<関連情報>
- https://news.ucsb.edu/2025/022019/ucsb-designed-soft-robot-intubation-device-could-save-lives
- https://www.science.org/doi/10.1126/scitranslmed.ads7681
迅速かつ自律誘導型挿管のためのソフトロボティクスデバイス A soft robotic device for rapid and self-guided intubation
David A. Haggerty, James R. Cazzoli, Marvin A. Wayne, Christopher J. Winckler, […] , and Elliot W. Hawkes
Science Translational Medicine Published:10 Sep 2025
DOI:https://doi.org/10.1126/scitranslmed.ads7681
Editor’s summary
Endotracheal intubation requires extensive training and clear anatomical visualization, making it challenging during emergencies, where first-pass failure rates are high. Here, Haggerty et al. developed a soft robotic device that guides a breathing tube into the trachea, reducing the need for extensive specialized training. Testing of the device by prehospital medical professionals showed the soft robotic device’s improved success and intubation duration compared with the gold-standard video laryngoscope. The findings suggest that this device could enable improved outcomes, broader use of intubation in emergency settings, and use by a broader segment of medical personnel and warrants further clinical evaluation. —Molly Ogle
Abstract
Endotracheal intubation is a critical medical procedure for protecting a patient’s airway. Current intubation technology requires extensive anatomical knowledge, training, technical skill, and a clear view of the glottic opening. However, all of these may be limited during emergency care for trauma and cardiac arrest outside the hospital, where first-pass failure is nearly 35%. To address this challenge, we designed a soft robotic device to autonomously guide a breathing tube into the trachea with the goal of allowing rapid, repeatable, and safe intubation without the need for extensive training, skill, anatomical knowledge, or a glottic view. During initial device testing with highly trained users in a mannequin and a cadaver, we found a 100% success rate and an average intubation duration of under 8 s. We then conducted a preliminary study comparing the device with video laryngoscopy, in which prehospital medical providers with 5 min of device training intubated cadavers. When using the device, users achieved an 87% first-pass success rate and a 96% overall success rate, requiring an average of 1.1 attempts and 21 s for successful intubation, significantly (P = 0.008) faster than with video laryngoscopy. When using video laryngoscopy, the users achieved a 63% first-pass success rate and a 92% overall success rate, requiring an average of 1.6 attempts and 44 s for successful intubation. This preliminary study offers directions for future clinical studies, the next step in testing a device that could address the critical needs of emergency airway management and help democratize intubation.