2025-11-20 ワシントン大学セントルイス校
<関連情報>
- https://source.washu.edu/2025/11/timing-may-be-key-to-effective-cancer-treatments/
- https://link.springer.com/article/10.1007/s11060-025-05242-3
MGMTプロモーターのメチル化と発現の概日変動は神経膠芽腫におけるテモゾロミドに対する感受性を予測する Circadian variation in MGMT promoter methylation and expression predicts sensitivity to temozolomide in glioblastoma
Maria F. Gonzalez-Aponte,Yitong Huang,William A. Leidig,Tatiana Simon,Omar H. Butt,Marc D. Ruben,Albert H. Kim,Joshua B. Rubin,Erik D. Herzog & Olivia J. Walch
Journal of Neuro-Oncology
Abstract
Purpose
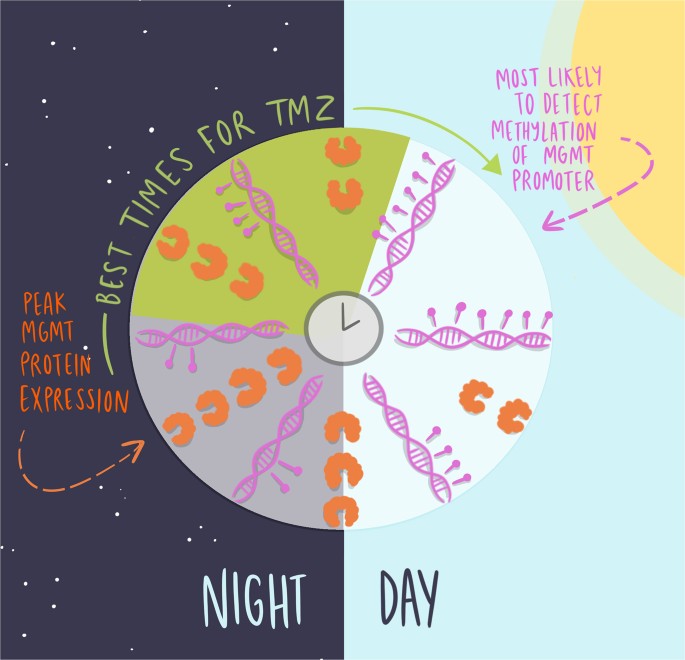
Recent studies show that glioblastoma (GBM) is more sensitive to temozolomide (TMZ) in the morning. In cells, inhibiting O6-Methylguanine-DNA-Methyltransferase (MGMT) abolished time-dependent TMZ efficacy, suggesting that circadian regulation of this DNA repair enzyme underlies daily TMZ sensitivity. Here, we tested the hypotheses that MGMT promoter methylation and protein abundance vary with time-of-day in GBM, resulting in daily rhythms in TMZ efficacy.
Methods
We assessed daily rhythms in MGMT promoter methylation in GBM in vitro and retrospectively analyzed MGMT methylation status in human GBM biopsies collected at different times of day. Next, we measured MGMT and BMAL1 protein abundances in GBM cells collected at four-hour intervals. To understand the therapeutic implications of circadian variations in MGMT, we incorporated its daily rhythms into an in vitro mathematical model capturing interactions between MGMT, TMZ, and GBM DNA.
Results
We found daily rhythms in MGMT promoter methylation and protein levels in GBM in vitro, and in patient biopsies peaking at midday. Further, MGMT protein levels peaked at CT4, corresponding to the time of maximal TMZ efficacy in vitro. When we incorporated cell-intrinsic circadian rhythms in MGMT protein into a mathematical model for GBM chemotherapy, we found that dosing when daily MGMT levels peaked and began to decline produced maximum DNA damage.
Conclusion
Our findings suggest that the likelihood of diagnosis of MGMT promoter methylation may vary with time of biopsy in GBM. Furthermore, theoretical modeling predicts that efforts to deliver TMZ after the daily peak of MGMT activity, with exact time being dose-dependent, may significantly enhance its therapeutic efficacy.
Graphical Abstract