2025-12-10 東京科学大学
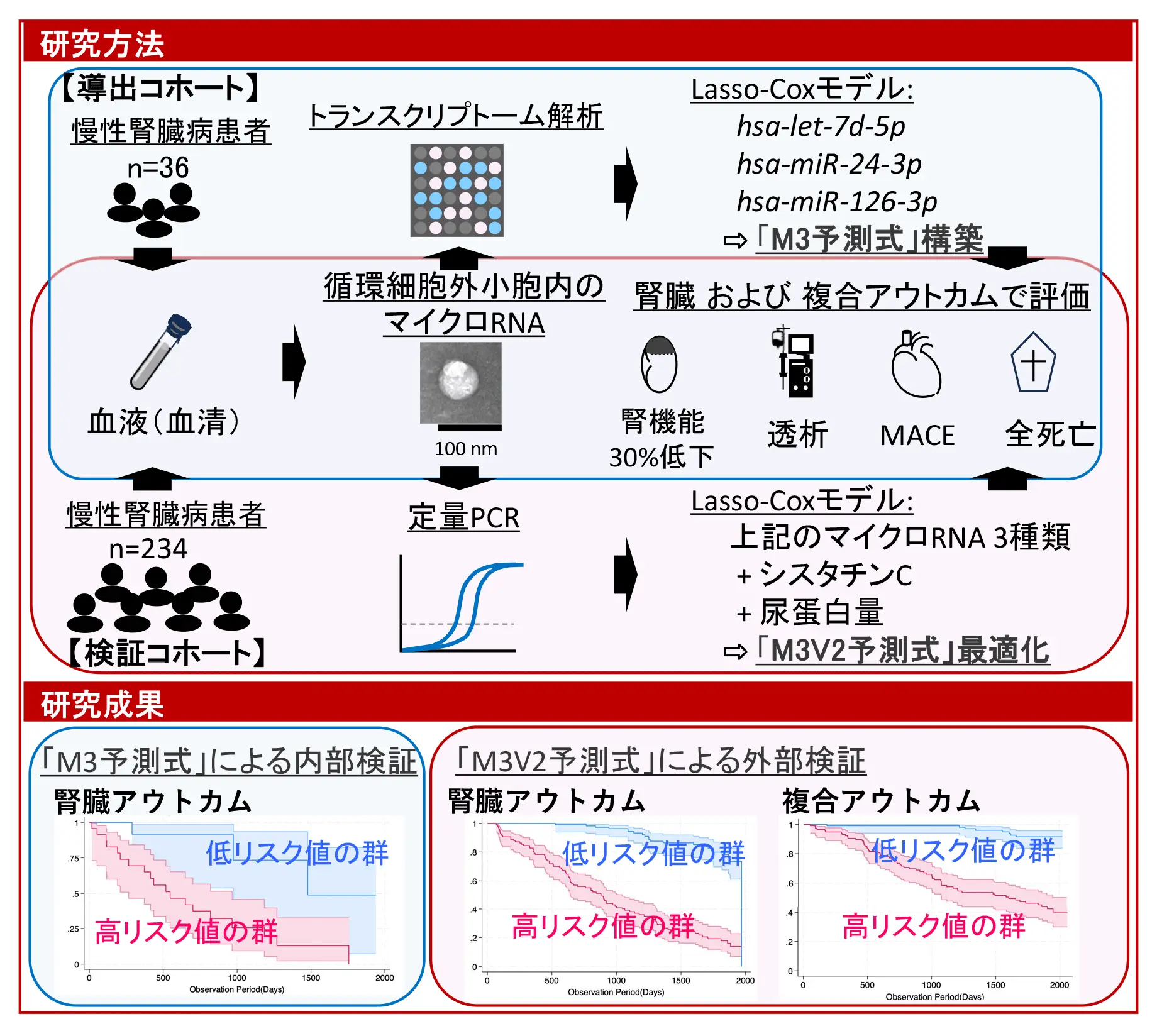
図1. 台風全体及び類型別の脳卒中リスク
<関連情報>
- https://www.isct.ac.jp/ja/news/8wgzygzwa34e#top
- https://www.isct.ac.jp/plugins/cms/component_download_file.php?type=2&pageId=&contentsId=1&contentsDataId=2820&prevId=&key=dc28faced6396f1b182af90e8b16e135.pdf
- https://www.sciencedirect.com/science/article/pii/S0160412025006579
熱帯低気圧曝露と脳卒中入院の関連性:日本全国における時系列分析 Association between tropical cyclone exposure and stroke hospitalization: A nationwide time-series analysis in Japan
Hisaaki Nishimura, Nobutoshi Nawa, Kiyohide Fushimi, Takeo Fujiwara
Environment International Available online: 5 November 2025
DOI:https://doi.org/10.1016/j.envint.2025.109906
Highlights
- Tropical cyclone (TC) exposure was associated with increased stroke hospitalizations.
- TC exposure was especially associated with an increase in hemorrhagic stroke.
- The first study to examine the association between TC exposure and stroke subtypes.
- Developing disaster-resilient healthcare systems is crucial.
Abstract
Background
Few studies have examined the association between tropical cyclone (TC) exposure and stroke hospitalization. This study aimed to clarify the association between exposure to TCs and emergency hospitalization for stroke.
Methods
Stroke hospitalizations were extracted from a nationwide administrative inpatient database for the period from May to October between 2011 and 2021. TC-exposed days were identified as those with TC-related peak sustained winds ≥ 15 m/s (30 knots). A time-series analysis was conducted to estimate the relative risks (RRs) of emergency hospitalization for stroke and its subtypes associated with TC exposure over lag 0–6 days.
Results
A total of 850,294 stroke hospitalizations were identified. TC exposure was associated with stroke hospitalization over lag 0–6 days (RR: 1.049 (95 % confidence interval (CI): 1.012–1.087)). On the day of exposure (lag 0 day), TC exposure was inversely associated with stroke (RR: 0.968 (95 %CI: 0.953–0.982)), while during lag 1–4 days, exposure to TCs was positively associated with stroke, with a maximum RR on lag 2 (1.031 (95 %CI: 1.023–1.038)). When stratified by stroke subtype, TC exposure was associated with hemorrhagic stroke (RR: 1.129, 95 %CI: 1.073–1.187), with increases in intracerebral hemorrhage (RR: 1.131, 95 %CI: 1.063–1.204) and subarachnoid hemorrhage (RR: 1.094, 95 %CI: 0.992–1.207), respectively. No TC-related increase in ischemic stroke was observed.
Conclusion
Exposure to TCs may increase the risk of stroke, especially hemorrhagic stroke.