2025-08-26 マックス・プランク研究所

Don’t open the letter. Many people avoid medical information out of fear of being overwhelmed, stigmatized, or because they don’t trust the healthcare system. © MPI for Human Development
<関連情報>
- https://www.mpg.de/25246796/avoidance-of-information-about-own-health
- https://academic.oup.com/abm/article/59/1/kaaf058/8229759
医療情報回避の有病率と予測因子:系統的レビューとメタ分析 Prevalence and predictors of medical information avoidance: a systematic review and meta-analysis
Konstantin Offer, MPhil, EdM , Natalia Oglanova, BSc , Lisa Oswald, PhD , Ralph Hertwig, PhD
Annals of Behavioral Medicine Published:10 August 2025
DOI:https://doi.org/10.1093/abm/kaaf058
Abstract
Background
Medical information avoidance—the prevention or delay of acquiring health-related information—is a growing concern for physicians, healthcare professionals, and policymakers. Yet, its prevalence and predictors have remained poorly understood.
Purpose
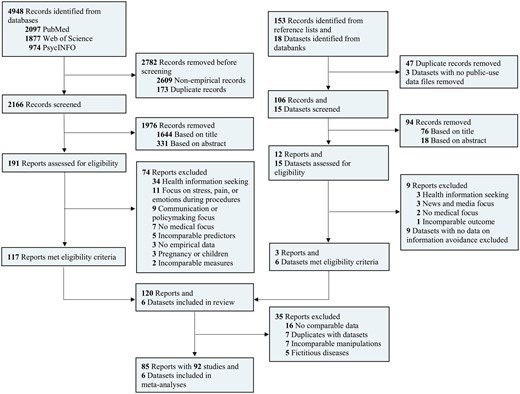
We conducted a systematic review and meta-analysis to clarify the prevalence and predictors of medical information avoidance, offering key insights into the worldwide empirical evidence.
Methods
We performed a systematic search, preregistered on the OSF and in accordance with PRISMA and MOOSE reporting guidelines. Additional individual participant datasets were obtained from the National Institutes of Health (NIH). Data analysis was performed using random-effects and mixed-effects models.
Results
A total of 92 studies and 6 individual participant datasets (564 497 unique participants, 25 countries) were analyzed. We found that almost 1 in 3 participants avoided or were likely to avoid information. Specifically, we estimated prevalence rates of 24% for diabetes, 29% for cancer, 32% for HIV, 40% for Huntington’s disease, and 41% for Alzheimer’s disease. We did not find any reliable association with gender or with race and ethnicity. Instead, we identified 16 significant predictors across cognitive, health-related, and sociodemographic domains. The strongest predictors were all cognitive: information overload (r = 0.26), perceived stigma (r = 0.36), self-efficacy (r = -0.28), and trust in the medical system (r = -0.25).
Conclusions
Nearly 1 in 3 participants avoided or were likely to avoid medical information. The highest prevalence rates were found for Huntington’s disease and Alzheimer’s disease, 2 incurable neurodegenerative diseases. Key cognitive predictors suggest entry points for policy interventions and future research.
Lay Summary
Medical information is more accessible than ever, but many people choose to avoid it. How common is this behavior, and what predicts it? To find out, we analyzed data from over 90 studies involving more than half a million people across 25 countries. We found that nearly 1 in 3 people avoided or were likely to avoid medical information. Avoidance was highest for incurable neurodegenerative diseases (Alzheimer’s disease: 41%, Huntington’s disease: 40%), moderate for severe but treatable conditions (HIV: 32%, cancer: 29%), and lowest for a chronic, manageable illness (diabetes: 24%). We identified 16 key predictors of medical information avoidance. Surprisingly, gender, race, and ethnicity were not among them. Instead, the strongest predictors were cognitive and emotional: mistrust in the medical system, feeling overwhelmed, low confidence in managing one’s health, and fear of being judged. Patterns of avoidance varied across world regions, suggesting that differences in healthcare systems may influence behavior. In this study, we do not judge whether medical information avoidance is good or bad. Instead, we offer the first comprehensive review of how common it is and what predicts it. More research is needed to understand the psychological and medical consequences of avoiding medical information.


