2025-09-18 名古屋大学,福島県立医科大学,九州大学,横浜市立大学,京都大学,東京大学,理化学研究所,科学技術振興機構,国立健康危機管理研究機構,千葉大学
<関連情報>
- https://www.jst.go.jp/pr/announce/20250918/index.html
- https://www.jst.go.jp/pr/announce/20250918/pdf/20250918.pdf
- https://www.science.org/doi/10.1126/scitranslmed.adv4214
COVID-19 mRNAワクチン接種後に測定された抗体価の経時的変化は、その後の感染リスクのある個人を特定できる Longitudinal antibody titers measured after COVID-19 mRNA vaccination can identify individuals at risk for subsequent infection
Hyeongki Park, Naotoshi Nakamura, Sho Miyamoto, Yoshitaka Sato, […] , and Masaharu Tsubokura
Science Translational Medicine Published:17 Sep 2025
DOI:https://doi.org/10.1126/scitranslmed.adv4214
Editor’s summary
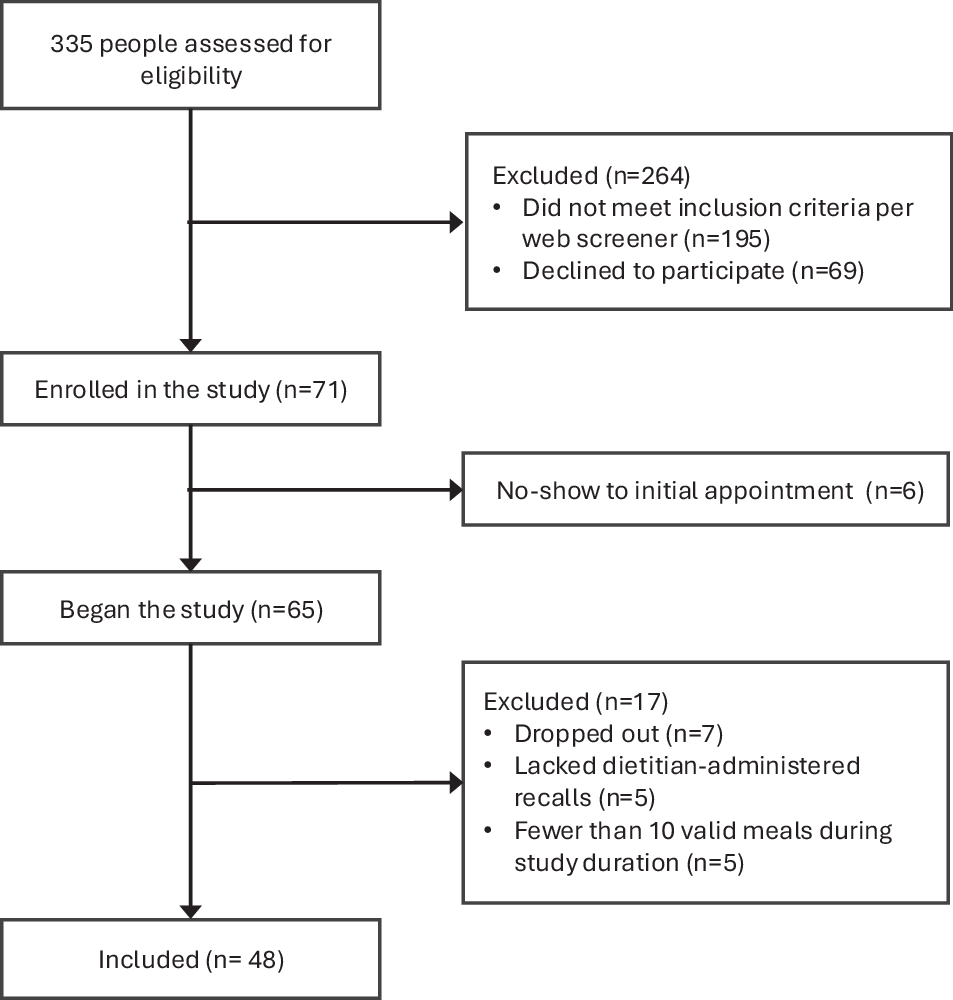
Determining who should receive booster vaccines for COVID-19 remains a priority as we progress into a postpandemic phase. Presently, those decisions are based on variables such as age and preexisting conditions, with no consideration of what a person’s immunity to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) looks like. Here, Park et al. asked whether immune dynamics could inform who may benefit from additional COVID-19 vaccine boosters. By analyzing antibody titers and T cell responses, the authors found that individuals could be binned into three stable populations, those with durable immunity, those with limited immunity (vulnerable), and those who started with robust immunity but experienced rapid waning (rapid-decliner). The authors then showed that those in the rapid-decline group were at risk for earlier SARS-CoV-2 breakthrough infection and that infection was associated with poor elicitation of SARS-CoV-2 spike protein–specific immunoglobulin A antibodies. Together, these data provide a landscape of SARS-CoV-2 vaccine responses that could provide guidance for prioritizing vaccine distribution. —Courtney Malo
Abstract
A key issue in the post–COVID-19 pandemic era is the ongoing administration of COVID-19 vaccines. Repeated vaccination is essential for preparing against currently circulating and newly emerging severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants. However, optimizing vaccination strategies is crucial to efficiently manage medical resources and establish an effective vaccination framework. Therefore, a strategy to identify poor responders with lower sustained antibody titers would be beneficial because these individuals should be considered high priority for revaccination. We investigated longitudinal antibody titer data in a cohort of 2526 people in Fukushima, Japan, collected between April 2021 and November 2022. Using mathematical modeling and machine learning, we stratified the time-course patterns of antibody titers after two primary doses and one booster dose of COVID-19 messenger RNA vaccines. We identified three populations, which we refer to as the durable, the vulnerable, and the rapid-decliner populations, and approximately half of the participants remained in the same population after the booster dose. The rapid-decliner population experienced earlier infections than the others. Furthermore, when comparing spike protein–specific immunoglobulin G (IgG) titers, spike protein–specific IgA titers, and SARS-CoV-2–specific T cell responses between participants who experienced subsequent infections after booster vaccination and those who did not, we found that spike protein–specific IgA titers were lower during the early stage after booster vaccination in participants who went on to become infected with SARS-CoV-2. This approach could be used to inform policy decisions on vaccine distribution to maximize population-level immunity both in future pandemics and in the post–COVID-19 pandemic era.