2022-11-10 ワシントン大学セントルイス
この知見は、2020年3月1日から2022年4月6日までに収集された、SARS-CoV-2感染1回の患者443,588人、2回以上の感染40,947人、非感染者530万人の米国退役軍人会(VA)のデータから導き出された。研究対象者の多くは男性であった。
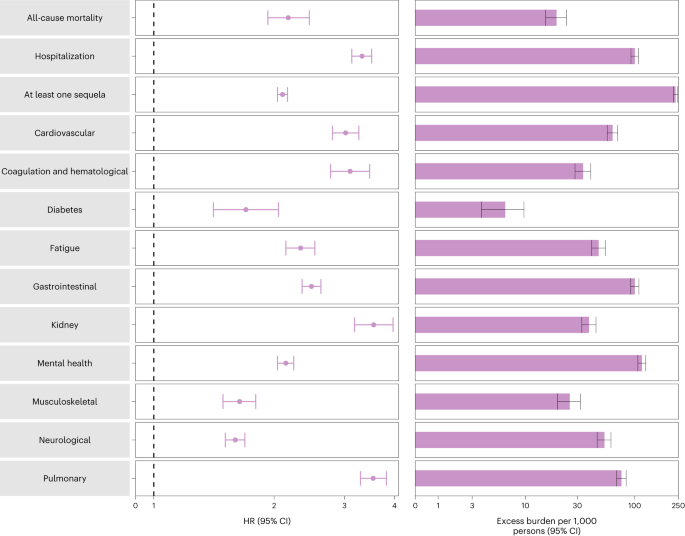
再感染者は、COVIDに1回だけ感染した人に比べて、死亡リスクが2倍以上、入院リスクが3倍以上となった。また、肺、心臓、血液、腎臓、糖尿病、精神衛生、骨と筋肉、神経障害などのリスクも高かったと、Nature Medicine誌に報告された。
この研究では、感染を繰り返した人は、1回しか感染しなかった人に比べて、肺の病気になる可能性が3倍以上、心臓の病気になる可能性が3倍以上、神経障害になる可能性が60%以上高かった。この高いリスクは再感染後の最初の1ヶ月で最も顕著に表れたが、6ヶ月後でもまだ明らかであった。
<関連情報>
- https://www.reuters.com/business/healthcare-pharmaceuticals/repeat-covid-is-riskier-than-first-infection-study-finds-2022-11-10/
- https://www.nature.com/articles/s41591-022-02051-3
SARS-CoV-2再感染に伴う急性期および急性期以降の後遺症について Acute and postacute sequelae associated with SARS-CoV-2 reinfection
Benjamin Bowe,Yan Xie & Ziyad Al-Aly
Nature Medicine Published:10 November 2022
DOI:https://doi.org/10.1038/s41591-022-02051-3
Abstract
First infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is associated with increased risk of acute and postacute death and sequelae in various organ systems. Whether reinfection adds to risks incurred after first infection is unclear. Here we used the US Department of Veterans Affairs’ national healthcare database to build a cohort of individuals with one SARS-CoV-2 infection (n = 443,588), reinfection (two or more infections, n = 40,947) and a noninfected control (n = 5,334,729). We used inverse probability-weighted survival models to estimate risks and 6-month burdens of death, hospitalization and incident sequelae. Compared to no reinfection, reinfection contributed additional risks of death (hazard ratio (HR) = 2.17, 95% confidence intervals (CI) 1.93–2.45), hospitalization (HR = 3.32, 95% CI 3.13–3.51) and sequelae including pulmonary, cardiovascular, hematological, diabetes, gastrointestinal, kidney, mental health, musculoskeletal and neurological disorders. The risks were evident regardless of vaccination status. The risks were most pronounced in the acute phase but persisted in the postacute phase at 6 months. Compared to noninfected controls, cumulative risks and burdens of repeat infection increased according to the number of infections. Limitations included a cohort of mostly white males. The evidence shows that reinfection further increases risks of death, hospitalization and sequelae in multiple organ systems in the acute and postacute phase. Reducing overall burden of death and disease due to SARS-CoV-2 will require strategies for reinfection prevention.